Doust’s journey with the asbestos-related cancer began in early 2016 when he experienced shortness of breath, or dyspenea. Wrongly diagnosed with pneumonia, he underwent a pleurodesis to remove excess fluid from around the lungs and was soon back to his exercise routine. Upon returning to Perth, he underwent another pleurodesis. He was told he had acute lymphatic leukemia and pleural mesothelioma.
Pleurodesis
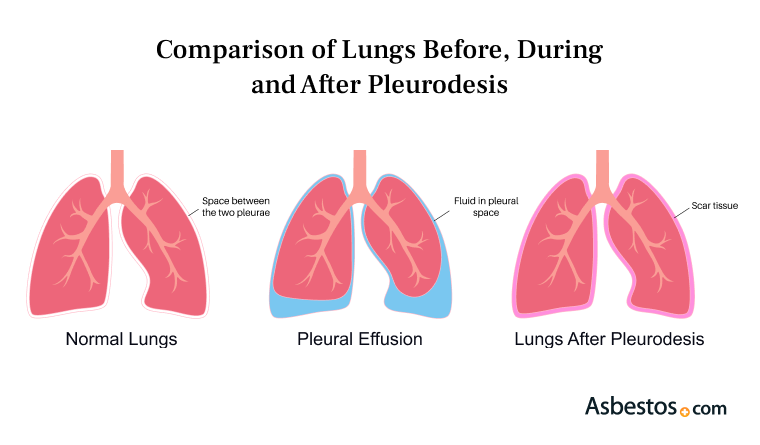
Pleurodesis is a surgical procedure that treats and prevents pleural effusions, a major complication of asbestos-related diseases such as pleural mesothelioma.

What Is Pleurodesis?
Pleurodesis is a procedure that obliterates the pleural space preventing fluid or air from building up. For instance, providers use mesothelioma pleurodesis as a palliative treatment to relieve symptoms. Pleurodesis may improve symptoms but is not intended to treat or cure the underlying cancer.
Pleurodesis creates scar tissue between the pleural lining of the lung and the chest wall. The scar tissue prevents fluid or air from building in the space and permanently prevents recurrent pleural effusion and pneumothorax.
The pleurodesis procedure closes and seals the pleural space in the chest wall where fluid can build up. This technique reduces the risk of pleural effusions, pneumonia and other chest complications.
Cancers that affect the pleural space (the space between the chest wall and the lungs) are frequently associated with a buildup of fluid called a pleural effusion. Other asbestos-related diseases are also associated with pleural effusion.
Pleural effusions can cause increased pressure on the lungs. Patients often experience shortness of breath, chest pain, cough and difficulty breathing while lying flat. If left untreated, pleural effusions can lead to infections.
- It can improve symptoms and quality of life in pleural mesothelioma patients
- It is less invasive and requires less recovery time than some treatments
- It prevents recurrent fluid buildup in many patients
- It can be done through a variety of different methods to meet unique patient needs
Who Qualifies for a Pleurodesis?
Some patients who have malignant mesothelioma or other conditions that may be indications for pleurodesis may not be candidates for the procedure. For pleurodesis procedures to be effective, the lung must be able to fully expand, so patients who have tumors so extensive that the lung cannot fully expand would not be candidates for the procedure.
A patient with a life expectancy of a few months or less may benefit from other palliative treatments for mesothelioma. These patients may not want to undergo the discomfort, hospitalization or other recovery requirements associated with pleurodesis surgery.
- Effusion causes symptoms for the patient, impairing quality of life
- Fluid recurs frequently, requiring drainage one or more times a month
- Patient should be in good overall health
- Prognosis of the patient should be at least 3 months
- Tolerability of the patient to general anesthesia and prolonged surgery
Providers most commonly use the pleurodesis procedure for malignant pleural effusions, but they may also use this procedure for recurrent non-malignant pleural effusions. Pleural effusions may occur for many reasons, including heart failure, kidney disease, liver disease, autoimmune disease and chronic lung disease. However, not every patient with these conditions needs pleurodesis.
Patients with localized cancer who are in good health may also choose a more aggressive treatment, such as pleurectomy/decortication, to remove the tumor. This type of surgery generally removes the pleural lining rather than just sealing it.

Types of Pleurodesis Procedures
Pleurodesis can be accomplished in a few different ways, including chemical, mechanical and rapid. No matter the type, the procedure generally involves a hospital stay of a few days. Researchers are studying newer techniques that may allow patients to go home the same day or the next day.
Patients usually receive medication prior to the procedure to help with pain and anxiety control. Before a pleurodesis procedure is completed, a provider will need to remove fluid in the pleural space. A drain usually accomplishes this.
After the provider drains the fluid, they must irritate the pleural lining to provoke inflammation and cause scarring, which fuses the two layers together. The two most common methods for inflammation between the layers of pleural lining are chemical and mechanical.
Chemical Pleurodesis
Talc is the most common agent used for chemical pleurodesis because it’s simple and cost-effective. The talc used for pleurodesis is medical grade, sterile and asbestos-free.
The choice of agent depends on several factors. These can include local expertise, availability of the chemical agent and the process for which the chemical pleurodesis is needed.
- Autologous blood
- Bevacizumab
- Bleomycin
- Cisplatin
- Corynebacterium parvum with parenteral methylprednisolone acetate
- Cytarabine
- Erythromycin
- Etoposide
- Fluorouracil
- Interferon beta
- Iodopovidone
- Mitomycin C
- Silver Nitrate
- Streptococcus pyogenes A3
- Talc
- Tetracyclines
During a chemical pleurodesis procedure, the surgeon performs a thoracoscopy, a procedure that puts a camera into the pleural space. The surgeon will then use a chest tube to insert powder, gas or a liquid form of the chemical being used to create the inflammatory reaction. Once the chemical has been distributed into the pleural space, the tube is removed.
Chemical pleurodesis are among the most common and effective methods for malignant pleural effusions. According to retrospective studies and systematic reviews, they may contribute to patient survival.
Mechanical Pleurodesis
Mechanical pleurodesis involves using a brush, pad or gauze to irritate the pleural lining rather than using a chemical to create inflammation. This procedure is also called dry abrasion.
Studies have shown similar outcomes between mechanical and chemical pleurodesis for recurrent pulmonary effusion. The medical team and patient should base the decision about which treatment modality to use on the prognosis and a discussion of the expected risks and benefits of each procedure.
Rapid Pleurodesis
Rapid pleurodesis is a procedure that uses a combination of a pleural catheter and chemical pleurodesis, usually talc pleurodesis. Rapid pleurodesis addresses one of the disadvantages of other pleurodesis procedures, namely the hospital stay required for recovery.
Rapid pleurodesis allows most patients to be discharged from the hospital within 48 hours of the procedure. Studies have shown that rapid pleurodesis protocols may be as effective as chemical pleurodesis in some cases.
Pleurodesis Recovery
Patients who undergo pleurodesis usually spend a few days in the hospital. The recovery process may take 2 to 7 days. After the procedure, fluid may continue to drain from the wound for 1 to 2 days. The bandage should stay on during this time.
After returning home, patients should rest when they feel tired and give themselves time to heal. The surgeon or healthcare team will recommend medication continuation, driving and when to return to normal activities, including work.
There are no specific dietary restrictions. Patients who experience an upset stomach from anesthesia may choose to eat bland foods until their stomach settles.
The medical team will also recommend how long to keep dressings, tape or sutures in place. Healthcare professionals generally advise avoiding swimming or soaking in a bath until 2 weeks after the procedure, but showering is generally allowed after 48 hours. The incision should be patted dry.
I had chest pain when I took a deep breath. I eventually had a biopsy and pleurodesis that provided the definitive diagnosis. Attitude counts for a lot, and willingness to pursue treatment adds up to a better chance for survival.
Pleurodesis Complications and Risks
The most common risks associated with pleurodesis are chest pain and fever. Some patients report shortness of breath or a feeling of tightness around the lungs, but they can usually alleviate this with medication before the procedure.
Fever is frequently associated with the inflammatory response that helps seal the pleural space. It may develop within a few hours of the procedure.
- Chest pain
- Fever
- Infection
Any surgical procedure carries a risk of infections. Generally, a medical team can treat infections with antibiotics. In very rare cases, pleurodesis can cause other complications, such as acute respiratory distress syndrome or cardiovascular complications.
Pleurodesis is a very successful procedure but is not always successful. Failure of the procedure is one possible risk.
Landmark Pleurodesis Mesothelioma Case
In September 2024, a jury granted $39 million to Bryce Zundel who underwent a pleurodesis procedure 2014 and was diagnosed with mesothelioma in 2021. He filed a lawsuit against the company that supplied the talc used in his procedure. This was the first lawsuit and verdict in a mesothelioma lawsuit over medical-grade talc used in a pleurodesis.
Zundel’s lawsuit claimed the talc Georgia-based Cimbar Performance Minerals supplied was contaminated with asbestos. The company imported the talc used in his procedure from China. During his pleurodesis, doctors injected sterile talcum powder around his left lung.
A Massachusetts judge cut the future pain and suffering amount awarded to Zundel 6 months after the verdict. The jury’s original award was $21.5 million. The judge reduced that to $6 million. The judge says the reduction from $39 million to more than $23 million is reasonable. The judge also upheld the jury’s original verdict.
Recommended Reading



