Raleen underwent a peritonectomy and later hyperthermic intraperitoneal chemotherapy. Her peritonectomy involved a 10-hour procedure during which multiple organs, portions of organs and as much of the cancer as possible were removed. Raeleen’s HIPEC procedure removed any remaining cancer cells and bathed her abdominal cavity with heated chemotherapy drugs.
Peritonectomy for Mesothelioma
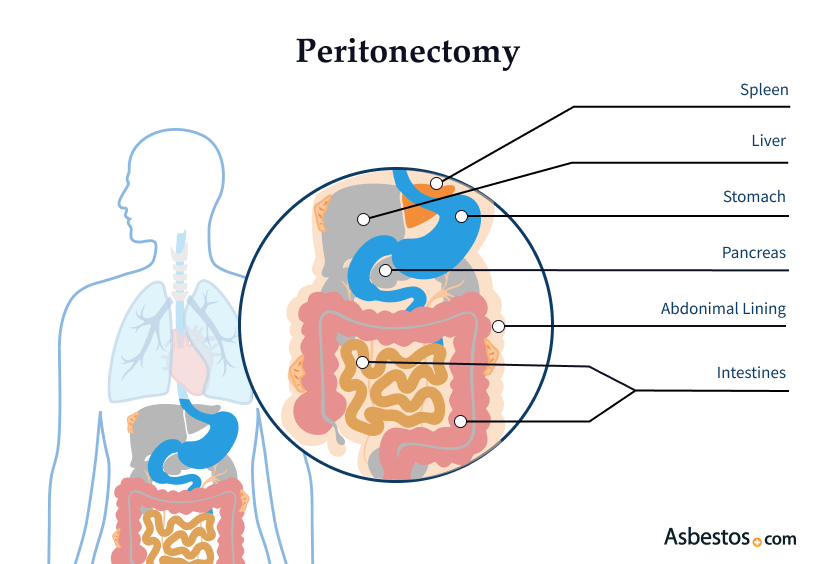
Peritonectomy is a cytoreductive surgery used to remove peritoneal mesothelioma tumors from a patient. This type of cancer affects the lining of the abdominal cavity. Following cytoreductive surgery, a heated chemotherapy bath (HIPEC) is commonly administered.
What Is a Peritonectomy for Mesothelioma?
Peritonectomy is a surgery used to treat peritoneal mesothelioma, a cancer that affects the lining of the abdominal cavity. The surgery involves removing the peritoneal lining affected by the cancer. It is often part of a larger treatment plan called cytoreductive surgery. This surgery is vital because it aims to remove as much tumor mass as possible.
Surgery may involve removing portions of various organs, including the stomach, intestines, liver, pancreas and spleen. After a peritonectomy, many patients receive heated intraperitoneal chemotherapy to target any remaining cancer cells.
- Peritonectomy with HIPEC can significantly improve survival rates for those with peritoneal mesothelioma.
- The procedure usually takes between 10 to 12 hours to complete, highlighting the complexity of the surgery.
- Patients typically remain in the hospital for several days after the surgery to monitor recovery and manage pain.
Dr. Charles Conway, a surgical oncologist at Ridley-Tree Cancer Center, explains, “Essentially, we remove the lining of the abdominal cavity…but also make sure we get all those surfaces where we know those mesothelioma cells are.”
A 2021 study in BJS Open looked at 40 mesothelioma patients who underwent peritonectomy. A total of 38 had a complete macroscopic tumor removal. Two patients had residual tumor nodules less than 2.5mm in size.
How Peritonectomy Works
Peritonectomy involves several steps and is performed under general anesthesia. This procedure aims to remove cancerous tissue and improve patient outcomes. During the surgery, the surgeon carefully removes the peritoneum affected by the tumor.
After the procedure, patients can expect to stay in the hospital for recovery. This recovery time allows the medical team to monitor vital signs and manage complications.
Cytoreduction is a complex procedure that generally lasts 10 to 12 hours. Because this mesothelioma surgery is so lengthy, patients are sometimes admitted to the hospital a day before the surgery. Doctors use the extra day for preoperative testing (X-rays, blood tests and other preparatory measures).
Tamron Little, a survivor of peritoneal mesothelioma, underwent a peritonectomy followed by HIPEC. She describes her experience as life-changing, emphasizing how the treatment significantly improved her health and quality of life.
Preparing for Surgery
Before having a peritonectomy, it’s essential to meet with the surgeon and their team. This meeting can be in person or online. It’s an opportunity for patients to learn more about the procedure and ask any questions they might have.
The surgical team will review all your medical records, imaging scans and biopsy results. This will confirm if you are eligible for a peritonectomy. They’ll also explain everything you need about preparing for surgery and recovery.
A few days before surgery, patients undergo several tests, including imaging scans and blood work. This ensures that the medical team clearly understands the tumor’s extent and the patient’s overall health.
Tumor Cytoreduction and Heated Chemotherapy
After removing the peritoneum, the surgeon may administer HIPEC. This treatment delivers heated chemotherapy directly into the abdominal cavity. The heat enhances the effectiveness of the chemotherapy, targeting any residual cancer cells left after the surgery.
This heated chemotherapy regimen – administered into the abdominal cavity for direct contact with cancer cells – is most commonly delivered after the tumor cytoreduction is complete. This generally lasts 90 minutes while the patient is still under general anesthesia.
Hospital Stay & At-Home Recovery
After surgery, patients can expect an extensive recovery period in the hospital and at home. Many patients have a post-op hospital stay of more than a week. While there, they can have chemotherapy as potentially curative care.
Once discharged from the hospital, patients should expect another two or three weeks of recovery at home. A large part of this depends on the digestive system’s recovery, which can experience significant complications after cytoreduction.
Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Who Is Eligible for a Peritonectomy?
Not everyone diagnosed with mesothelioma is a candidate for a peritonectomy. Eligibility depends on several factors. Doctors consider the tumor stage, the patient’s overall health and the disease’s extent.
Patients with early-stage peritoneal mesothelioma often qualify for the surgery. Those with localized tumors are the best candidates, as they are more likely to benefit from the procedure. Additionally, patients should have good overall health to tolerate the long surgery and recovery process.
A thorough consultation with a mesothelioma specialist is crucial. They can provide insights into whether peritonectomy is a suitable option based on the individual’s situation.
Benefits of Peritonectomy Surgery for Peritoneal Mesothelioma
Peritonectomy is a leading treatment for peritoneal mesothelioma due to its potential benefits. One of the primary advantages of this surgery is its ability to remove cancerous growths from the abdominal cavity. By targeting the tumors directly, peritonectomy aims to extend life expectancy for many patients.
Many survivors have shared their positive experiences after undergoing this surgery. For instance, Raleen highlights how her life changed after the procedure. She felt renewed hope and could resume many of her daily activities.
Additionally, studies have shown that peritonectomy, especially when combined with HIPEC, can lead to improved survival rates. Patients often experience relief from symptoms and a better quality of life after the surgery.
Peritonectomy Risks and Complications
Like all surgeries, peritonectomy carries certain risks. Patients need to understand these before undergoing the procedure. Some common surgical risks include:
- Infection: As with any surgery, there is a risk of infection at the surgical site.
- Bleeding: Significant bleeding can occur during or after surgery, requiring blood transfusions or additional procedures.
- Anesthesia Complications: There are potential complications associated with general anesthesia, although these are rare.
After HIPEC, patients may experience side effects such as abdominal discomfort and fatigue. These side effects are temporary and can be managed with medication and rest.
How Does a Peritonectomy Affect Life Expectancy and Prognosis?
Mesothelioma experts consider peritonectomy surgery critical to treating peritoneal mesothelioma. A combination of cytoreductive surgery and chemotherapy can help some patients become long-term survivors. In general, when peritoneal mesothelioma patients follow this treatment regimen, doctors report a median survival of approximately three years.
One study in the Medscape Journal of Medicine of 49 patients achieved a median survival of 92 months (about 7.5 years). This differs drastically from the typical mesothelioma prognosis of one year or less.
If you have peritoneal mesothelioma, proper treatment may help you become a survivor. Treatments such as cytoreduction may add years to your lifespan. Discuss your situation with a mesothelioma specialist and create a personalized treatment plan.
Common Questions About Peritonectomy Surgery
- What are the chances of mesothelioma returning after a peritonectomy?
-
The risk of recurrence varies based on individual factors, including the tumor’s characteristics and how much was removed during surgery.
- Is a peritonectomy always combined with HIPEC?
-
While it is common to combine the two, it may not be necessary in every case. The treatment plan is tailored to the patient’s specific needs.
- How does peritonectomy compare to other treatments for peritoneal mesothelioma?
-
Peritonectomy is often more aggressive than chemotherapy alone, targeting the cancer directly in the abdominal cavity.
- What lifestyle changes will I need to make after peritonectomy surgery?
-
Patients may need to adjust their diet and activity levels during recovery. Following the doctor’s recommendations is essential for a successful recovery.
- Are there any alternative treatments if I’m not a candidate for peritonectomy?
-
Yes, options like chemotherapy, palliative care, and clinical trials may be available for patients who do not qualify for surgery.




