
75 Francis St, Boston, MA 02115
Year Built: 1832
Number of Beds: 793 beds
Number of Physicians: 4
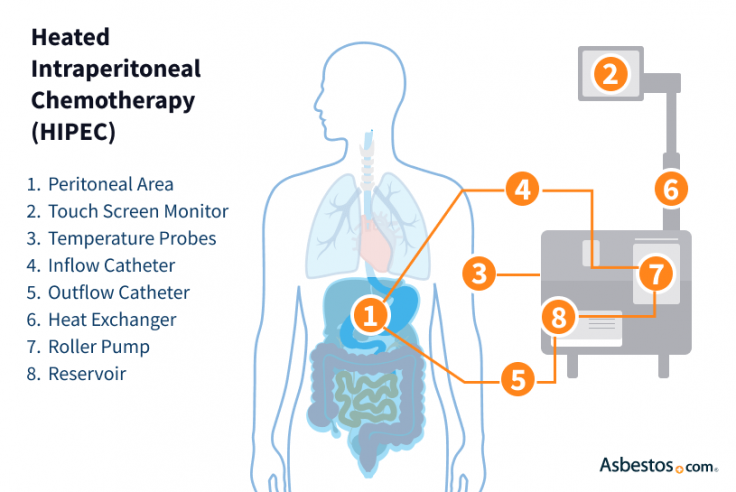
HIPEC (hyperthermic intraperitoneal chemotherapy) is a procedure used to treat peritoneal mesothelioma. Cytoreductive surgery is used to remove malignant tumors from the abdominal cavity. The area is then bathed with heated chemotherapy drugs to target the remaining cancer cells.
HIPEC, which stands for hyperthermic intraperitoneal chemotherapy, is the second part of a 2-step procedure to treat peritoneal mesothelioma. This process combines surgery with a warm chemo wash.
After tumor-removing surgery, heated liquid chemo is applied directly, filling your belly. Also known as “hot chemo,” HIPEC aims to kill any mesothelioma cells that could remain after surgery.
Key Facts About HIPEC for Mesothelioma
The goal of HIPEC is to treat peritoneal mesothelioma more effectively by delivering chemo directly where it’s needed most. This approach allows doctors to kill microscopic cancer cells left behind after surgery without affecting the entire body.
HIPEC combines cytoreductive surgery with a heated chemotherapy solution to treat mesothelioma. The surgery removes visible tumors. The heated chemo helps kill cancer cells that may remain in the abdominal lining.
Heating the chemo causes blood vessels to expand and improves drug absorption. It also allows doctors to use higher doses than systemic or whole-body chemo without harming healthy cells throughout your body. The entire HIPEC process takes 6-8 hours to complete.
Cytoreductive surgery is the first step of the HIPEC process. Surgeons remove all visible signs of peritoneal mesothelioma in your abdominal cavity. This may include parts of the lining around the organs in your abdomen called the peritoneum, as well as the spleen, bowel or other affected tissue. This process is called a peritonectomy.
Removing as much of the cancer as possible is key to improving outcomes. Surgeons aim to leave behind no visible tumor before moving on to HIPEC.
Once tumors are removed, surgeons begin HIPEC. They pump heated chemo drugs such as cisplatin or mitomycin C into your abdomen. The chemo circulates for about 90 minutes using a perfusion machine that keeps the solution warm and gently moving.
How HIPEC Works
While the chemo circulates, surgeons agitate the abdomen to help the solution reach every surface. This process is sometimes called “shake and bake” among surgeons and patients.
Dr. Jason Foster, a surgical oncologist, compares the process to cleaning: “It’s like combining your power washer with the vacuum cleaner at home. Sometimes, you have to scrub the stain out, then go back over with the vacuum.” After the chemo is drained, surgeons finish the procedure and begin closing the incisions.
We coordinate your care with top cancer centers and guide you through every step.
Get Help NowPeritoneal mesothelioma patients often have questions about what to expect before, during and after HIPEC. The process includes preparation, hospital recovery and at-home healing.
From Prep to HIPEC Recovery
Recovery is different for everyone. Some patients may feel fatigued, while others regain strength quickly. It’s important to follow your mesothelioma care team’s instructions closely.
HIPEC offers many benefits for treating peritoneal mesothelioma. Because it targets the cancer site directly, it can improve survival while reducing whole-body side effects. Only 1 chemo session is needed during surgery, and it allows for higher drug doses in the abdominal cavity. Plus, systemic side effects are lower than with traditional chemo.
Dr. Edward Levine studied 46 patients with peritoneal mesothelioma who had cytoreductive surgery with HIPEC. Although physical and emotional well-being declined 3 months post-surgery, quality of life returned to baseline by 6 months and continued to improve over the next 18 months.
Success Rate of HIPEC for Mesothelioma
The March 2025 report on the Indian Network for Development of Peritoneal Surface Oncology and Indian Society of Peritoneal Surface Malignancies conducted a consensus exercise. The report states: “Hundred percent panelists agreed that CRS-HIPEC should be the standard-of-care for newly diagnosed PeM [peritoneal mesothelioma] if the disease is completely resectable, and there is no contraindication to surgery.”
As Dr. Jonathan Foster explains, “Patients want to feel they have done everything they possibly can to fight this battle. Surgery with HIPEC is an important tool. It appears to be one therapy that can get people to this curative state.”
Like any mesothelioma surgery, HIPEC has side effects. Not everyone experiences them, and most are manageable with proper care and treatment.
Common Side Effects
More serious risks are similar to those associated with other intensive surgeries. These risks may include infection, bleeding or damage to nearby organs. Peritoneal mesothelioma patients may also experience blood clots, and in rare cases, develop a fistula (abnormal connection) connecting the intestines to other structures. However, most people recover well with proper monitoring and care.
Managing side effects starts with preparation and continues through recovery. For many people with peritoneal mesothelioma, the most challenging aspect of HIPEC recovery is fatigue. It may take several months until you feel back to normal. Until then, staying active within your limits and maintaining a balanced diet to keep your energy levels up is essential.
Tips for Managing HIPEC Side Effects
If you develop any worsening side effects or conditions, call your mesothelioma doctor to discuss ways to manage or treat them. For example, a wound infection requires antibiotics and should be treated quickly.
As peritoneal mesothelioma survivor Tamron Little shares, “The way I managed it was by taking my pain medication at the prescribed scheduled times. I also carried a small pillow around with me. I would place the pillow right on my stomach and just hold it there.”
HIPEC is most effective for people with peritoneal mesothelioma that hasn’t spread outside the abdomen. Mesothelioma doctors look at several factors to decide eligibility. Cancer must not be beyond the abdominal cavity, meaning no distant metastasis exists. You should also be in good overall health with an acceptable performance status. You must also have no severe heart, kidney or lung issues.
Consulting a mesothelioma specialist is key. They can help determine if HIPEC is right and explain what to expect based on your cancer stage.
HIPEC is offered to peritoneal mesothelioma patients at several top cancer centers across the United States. Treatment typically begins with a referral or consultation with a surgical oncologist.
Our Patient Advocates can help connect you with HIPEC specialists, schedule appointments and assist with insurance paperwork. Ask about which hospitals offer HIPEC for mesothelioma and how our team can support you.

75 Francis St, Boston, MA 02115
Year Built: 1832
Number of Beds: 793 beds
Number of Physicians: 4

3855 Health Sciences Dr., La Jolla, CA 92093
Year Built: 1979
Number of Physicians: 2

12902 Magnolia Drive, Tampa, FL 33612
Year Built: 1986
Number of Beds: 206 beds
Number of Physicians: 10

1 Gustave L. Levy Pl New York, NY 10029
Year Built: 1855
Number of Beds: 1,144 beds
Number of Physicians: 3

620 Howard Ave, Altoona, PA 16601
Year Built: 2013 (became part of UPMC)
Number of Beds: 380 beds
Number of Physicians: 1

1514 Jefferson Hwy, Jefferson, LA 70121
Year Built: 1983
Number of Beds: 473 beds in main hospital
Number of Physicians: 4
Some patients may need additional chemotherapy after HIPEC based on cancer staging or if the disease returns. Systemic chemotherapy can help treat cancer cells that may be outside the abdominal cavity. Your doctor will determine the need based on follow-up imaging and lab results.
HIPEC is usually done only once, but it may be repeated in select cases where the disease returns and the patient is healthy enough for more surgery. Repeat HIPEC procedures are more complex and depend on prior treatment history. A mesothelioma specialist can help assess if a second procedure is possible.
Top cancer centers in the U.S., such as MD Anderson, UCSF and the University of Chicago, offer HIPEC for peritoneal mesothelioma. These hospitals have experienced surgical oncologists and dedicated care teams. Working with a center that specializes in mesothelioma is important for achieving the best results.
Patients may experience pain or discomfort after surgery, but pain is usually well-controlled with medication. Most patients describe the discomfort as manageable and temporary. The care team works closely with patients to ease symptoms and support recovery.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2025, November 5). HIPEC and Cytoreductive Surgery for Mesothelioma. Asbestos.com. Retrieved February 5, 2026, from https://www.asbestos.com/treatment/chemotherapy/hipec/
Selby, Karen. "HIPEC and Cytoreductive Surgery for Mesothelioma." Asbestos.com, 5 Nov 2025, https://www.asbestos.com/treatment/chemotherapy/hipec/.
Selby, Karen. "HIPEC and Cytoreductive Surgery for Mesothelioma." Asbestos.com. Last modified November 5, 2025. https://www.asbestos.com/treatment/chemotherapy/hipec/.

Surgical oncologist and peritoneal specialist Dr. W. Charles Conway is director of surgical oncology at the Ridley-Tree Cancer Center in Santa Barbara, California. He specializes in gastrointestinal cancers and peritoneal surface malignancies, including mesothelioma.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
