Mesothelioma Treatment Uses Natural Immune Cells
Research & Clinical TrialsWritten by Sean Marchese | Edited by Walter Pacheco
For patients with mesothelioma cancer, immunotherapy is a promising new field. Results from a recent study at Rice University in Houston are exciting. Researchers are looking at ways the natural immune system can help fight this cancer.
The study examined the therapeutic effects of interleukin 2, a form of immunotherapy for mesothelioma. IL2 is a protein that regulates white blood cells. It does this through cytokines, a type of signal that affects other cells.
Researchers studied these effects in mice. After one week of treatment the tumor burden in the mice fell 80%.
“This study provides support for the clinical evaluation of this IL2-based delivery system,” the authors wrote. Continued research with IL2 treatments in humans could lead to a new standard for mesothelioma therapy.
Using Cytokines Increases Effectiveness
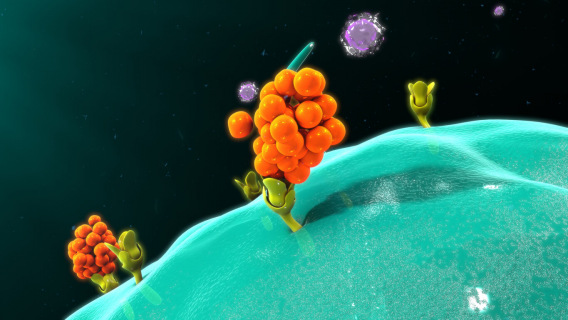
Cytokine factories are delivery systems that invoke innate immune cells to fight tumors. Each drug “factory” consists of thousands of drug-producing cells contained in a microscopic gel-like bead. The study investigators used mice to model the efficacy of IL2 cytokine factories.
“The rapid clinical course of malignant mesothelioma necessitates the development of highly effective treatment modalities that are safe and fast-acting,” the researchers wrote. These factories enabled 150 times higher IL2 concentrations in localized areas.
“IL2 cytokine factories led to the eradication of aggressive mouse malignant mesothelioma tumors and protection from tumor recurrence,” the authors concluded. Almost 90% of mice treated with at least 1.5 μg survived more than twice as long as mice that did not receive treatment.
After one week of treatment, tumor reduction in 19 of 26 mice was greater than 45% percent, regardless of the dose. More than 91% of mice treated with at least 2.5 μg had a greater than 75% reduction in tumor burden in one week. All mice treated with 5 μg had a 90% reduction in tumor burden.
Interleukin 2 Activates the Immune System
IL2 is one of the only cytokine cancer therapies the FDA has approved and is critical in activating the immune system against infection and disease. The mouse model used in the study demonstrated improvements to the IL2 delivery system.
IL2 immunotherapy creates a rapid response of T cells. These immune cells destroy tumor cells and develop antibodies against recurrence. Delivering IL2 via a cytokine factory is beneficial for patients who have not responded to other immunotherapies.
The researchers could control IL2 dosing through the density of engineered cells suspended in capsules. They found that as the cell concentration per capsule increased, the amount of released IL2 also increased. The method provided dose-dependent control without loss of cell viability.
The study authors noted they did not observe any significant deviations in body weight over time. This suggests that the therapy was well tolerated. The authors also noted that the treatment increased the effectiveness of anti-PD1 checkpoint therapy.
Benefits for Pleural and Peritoneal Patients
The data suggests that this therapy has the potential to be a safe and effective treatment for mesothelioma patients. Feasibility for both peritoneal mesothelioma and pleural mesothelioma was tested.
To test the feasibility for peritoneal patients, researchers implanted the therapy in the intraperitoneal space in mice. IL2 cytokine factories require only limited access to the target site.
In pleural testing, researchers found the local concentration was at least 100 times greater than the systemic concentration, or whole body concentration. This is critical for reducing the side effects as medication “leaks” out of the cancer region.
Precautions were taken to test toxicity in the liver, kidney and lungs. IL2 therapy can often cause adverse effects in these systems. They found no significant cellular changes in any of these organs at the end of their study. The treatment also did not show substantial effects on insulin or glucose levels.
Findings suggested that extended treatment wouldn’t pose a safety issue to patients. The results showed that the capsules didn’t continue to deliver cytokines after treatment completion. The dosage concentration peaked by day four and declined as scar tissue formed on the capsule. More than 80% of the capsules could be retrieved, highlighting the stability of the cytokine factories at body temperatures.
Importance of Clinical Trials
While the authors noted that their results suggest “that the cytokine factories were well tolerated by the host immune system,” this study took place in mice. Drug safety testing is necessary before clinical use.
The Rice University researchers highlighted ways that the treatment could translate to a clinical setting. In the study, they examined the feasibility of dosing in multiple locations.
Because pleural mesothelioma, for example, has a 5-year survival rate of less than 10%, researchers underscored the importance of promising treatment for this aggressive and rare cancer. “The continued occurrence of malignant mesothelioma necessitates the clinical assessment of new, effective treatments,” researchers noted.
Asbestos exposure is the primary cause of mesothelioma, which can develop in the chest, abdomen, heart or testes. The current standard of treatment includes surgery, chemotherapy and radiation. “The potential of the IL2 cytokine factory described here to ease the global burden of malignant mesothelioma highlights the urgency of its evaluation in clinical trials,” the authors concluded.







