Baylor Study: Mesothelioma ‘Staged Surgical Approach’ Increases Survival
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco

Select patients diagnosed with mesothelioma cancer in both the thoracic and abdominal cavities still can achieve an extended survival if their treatment center performs the preferred types of aggressive surgery, according to a recent study at Baylor College of Medicine in Houston.
Patients undergoing bicavitary cytoreductive surgery that includes the lung-sparing, extended pleurectomy and decortication had a median survival of 58.2 months, the study found. The Journal of Thoracic and Cardiovascular Surgery published the results online in December.
“Long-term survival can be achieved with an aggressive, staged surgical approach,” study authors wrote. “For patients with localized disease that is amenable to multimodality therapy with resection, prolonged survival can be achieved.”
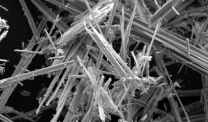
Mesothelioma is a rare and aggressive cancer that is caused by exposure to asbestos. It typically comes with a poor prognosis and is rarely diagnosed in both the chest and the abdomen.
Aggressive mesothelioma surgery in one cavity can be overwhelming, and having two back-to-back surgeries is almost unheard of outside of select mesothelioma specialty centers such as Baylor.
“Reports of bicavitary CRS [cytoreductive surgery] are limited,” the authors wrote. “Our series is the only non-case report of patients who underwent staged resection of chest and abdominal mesothelioma.”
Mesothelioma Surgeries Produced Different Results
From 2014 to 2021, 440 patients with mesothelioma were evaluated at Baylor College of Medicine. Only 14 of those (3%) underwent the two-stage chest and then abdominal operations. Of the 14 bicavitary patients, eight underwent the extended pleurectomy decortication and six had the extrapleural pneumonectomy.
For the abdominal surgery that followed, all 14 underwent a standard peritonectomy and hyperthermic intraperitoneal chemotherapy, another specialty procedure known as HIPEC.
Six of the patients received chemotherapy between the two operations and five received adjuvant chemotherapy after each operation.
Median overall survival, for the entire cohort, was 33.6 months, with a five-year survival rate of 20%.
The objective of the retrospective study was to determine whether the latest extended pleurectomy decortication surgery or the older, lung-sacrificing extrapleural pneumonectomy was more effective as part of bicavitary resection. The results were not even close.
From the date of the second surgery, median overall survival was only 13.5 months for those undergoing the EPP, but 58.2 months for those having the extended P/D. The median progression-free survival was 12.9 months vs. 26.3 months for EPP and ePD groups, respectively, following the first surgery.
Dr. David Sugarbaker Pioneered EPP Surgery
Results of the study are one reason Baylor – like many specialty centers treating mesothelioma –has moved away from the once-groundbreaking EPP surgery that was made popular by the heralded thoracic surgeon and mesothelioma specialist Dr. David Sugarbaker.
Sugarbaker, who became known as Mr. Mesothelioma during his more than two decades at Brigham and Women’s Hospital in Boston, came to Baylor Medical Center in 2014 as director of The Lung Institute. He died in 2018.
“The choice of operative procedure reflects a shift from EPP to ePD in our institution that is similar to many mesothelioma centers,” authors wrote. “EPD is now our standard approach for the majority of patients.”
Earlier studies involving only pleural mesothelioma in the thoracic cavity had shown similar survival times when comparing the two surgeries, but a quicker recovery and a lower morbidity rate with the ePD.
In this study, there were no immediate deaths following the first surgery, and all 14 patients proceeded to the second surgery. There were two patients – both starting with the EPP – who died within 90 days of the abdominal surgery.
“When considering bicavitary cytoreductive surgery for mesothelioma, we would recommend only performing ePD and avoiding EPP in this cohort of patients,” authors concluded.
Baylor Medical Center thoracic surgeon Dr. R. Taylor Ripley was the lead author of the study. One of the co-authors was surgical oncologist Dr. Paul Sugarbaker, brother of Dr. David Sugarbaker and a pioneer in advancing treatments for peritoneal mesothelioma. He last served at MedStar Washington Hospital Center.