Orphan Drug Designation Given to New Mesothelioma CAR T-Cell Therapy
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco
In early 2023, the world-class Hospital of the University of Pennsylvania will open a groundbreaking clinical trial for mesothelioma patients utilizing a next-generation immunotherapy with a novel delivery platform.
The U.S. Food and Drug Administration cleared the path in September by granting orphan drug designation for SynKIR-110, a CAR T-cell therapy designed to target solid tumors expressing a specific protein typically found in mesothelioma cancer.
By granting the orphan drug designation, the FDA can provide financial incentives such as tax credits for clinical trials and seven years of market exclusivity. It is designed to help find answers for treating rare diseases or disorders that affect fewer than 200,000 people in the U.S.
A first-in-human clinical trial, officially known as STAR-101, will be assessing preliminary efficacy, tolerability and safety after showing impressive results – including complete remissions – in earlier murine (rodent) models.
As part of the clinical trial, SynKIR-110 also will be used on patients with bile duct (cholangiocarcinoma) and ovarian cancer, but only those expressing the cell-surface protein mesothelin.
SynKIR-110 is a product of Verismo Therapeutics, a Philadelphia-based biotechnology company that has built the KIR-CAR delivery platform, a modified killer-like receptor designed to improve efficacy and persistence against aggressive solid tumors. It will be the first product to use the KIR-CAR platform.
“There is a high unmet need for a successful treatment option [for mesothelioma],” Dr. Bryan Kim, co-founder and chief executive officer at Verismo, told The Mesothelioma Center at Asbestos.com. “Once we demonstrate this can be used safely in patients, it opens a whole new field of potential targets and diseases we can treat using our novel KIR-CAR technology.”
Researchers Still Looking for T-Cell Therapy Success
Although T-cell therapy has been especially effective with blood cancers such as leukemia and lymphoma, it has been generally ineffective to this point against advanced-stage solid tumors like mesothelioma.
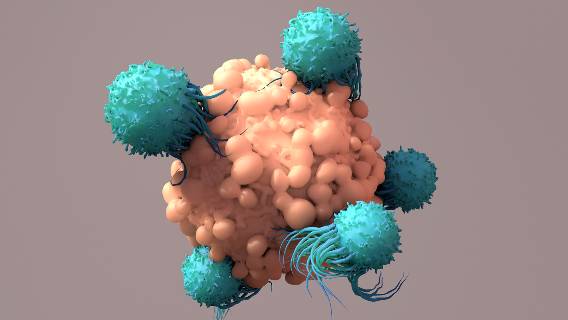
T-cell therapy is often based upon a patient’s unique genetic profile and the laboratory modification of their T cells, a type of white blood cell responsible for protecting the body against disease and infection.
Some cancer cells, though, avoid the immune response by using surface proteins such as mesothelin to trick T cells into leaving them alone. T cells can be modified in a laboratory to better recognize the cancer and attack it.
“One of the hurdles that T-cell therapies face when treating solid tumors is that T cells become terminally differentiated and more exhausted in the harsh tumor environment,” Kim said. “This exhaustion results in T cell failure. The novel way we’ve gone about addressing the exhaustion is by building the cells with a multichain structure that includes components found on natural killer cells.”
More Effective Mesothelioma Therapies Needed
The need for more effective treatments is obvious for solid tumors expressing mesothelin, the cell-surface protein. The five-year survival rate is 50% for ovarian cancer, just 30% for cholangiocarcinoma and only 10% for mesothelioma, according to Verismo.
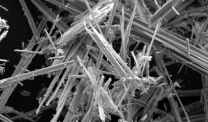
Mesothelioma, which is caused almost exclusively by an exposure to toxic asbestos fibers, is diagnosed in an estimated 3,000 people annually within the U.S. Although a multimodality approach that includes mesothelioma surgery often works bests, less than a third of those diagnosed even qualify. Too often, mesothelioma is not diagnosed until later stages, and only chemotherapy is advised.
“This will be the pivot point for over a decade of work that has gone into developing our novel KIR-CAR T platform, where we can finally transition from seeing it work in preclinical models to using it to treat patients in need,” Kim said.