Study Suggests Relationship Between Stromal Tumors and Mesothelioma
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco
Early identification of peritoneal mesothelioma cancer – when it is most effectively treated – may become more common after a recent study revealed a potential link to gastrointestinal stromal tumors.
A single-center retrospective review by the division of surgical oncology at University of California San Diego Moores Cancer Center identified a previously underrecognized, synchronous co-occurrence between the two rare diseases.
Annals of Surgical Oncology published the case series in July, which found that one in every 17 patients undergoing resection for gastrointestinal stromal tumors, known as GISTs, also had peritoneal mesothelioma cells nearby.
“There is certainly more work to be done in terms of better understanding the relationship,” surgical oncologist and co-author Dr. Jason Sicklick, GIST specialist, told The Mesothelioma Center at Asbestos.com. “I can’t say exactly where this will lead, but it’s more important now on the diagnostic side of things.”
The authors noted that the potential relationship between the two also could have an effect on future adjuvant therapy.
Rare Cancers Found in Close Proximity
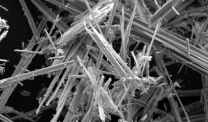
GIST is a cancer that forms in the stomach and small intestines, indicated by a growth of nerve cells into the walls of organs. In the U.S. it is found in an estimated seven people per million and thought to be genetically caused.
Although earlier studies have shown that 14% to 33% of GISTs occur in patients with other malignancies, the relationship with mesothelioma has never been seriously explored.
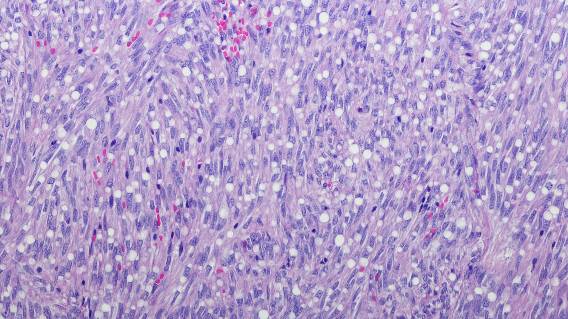
Peritoneal mesothelioma is an even rarer abdominal cancer, found in an estimated two cases per 1 million people annually in the U.S. Mesothelioma is typically caused by the inhalation or ingestion of toxic asbestos, and is more likely to occur in people with the BAP-1 gene mutation.
The retrospective review at Moores Cancer Center involved 137 patients from 2010 to 2021 who underwent GIST resection. During surgery, eight of those patients were found to have peritoneal mesothelioma, only one of which had been previously diagnosed. All tumors were removed surgically.
At a median follow-up of 14 months, all eight were without GIST recurrence. Seven of the eight – those with papillary mesothelioma – remained without recurrence. One patient with malignant mesothelioma was diagnosed with recurrence after five months, even after cytoreduction and hyperthermic intraperitoneal chemotherapy treatment.
“Mesothelioma was one of the cancers that exhibited increased co-occurrence both before and after GIST diagnosis,” the authors wrote. “The high co-occurrence rates of GIST and PM relative to the independent incidence of each one suggest the potential for a local, nonindependent symbiotic relationship.”
GIST, Mesothelioma Relationship Likely Underreported
Median age of the patients with GIST diagnosis was 57 years. Seven of the eight were clinical patients of Sicklick’s. Four of the eight had a history of other malignancies or benign tumors. In six of the eight patients, the mesothelioma nodules were found close to the GISTs.
The authors believe the high percentage of co-occurrence of GIST and mesothelioma has been underreported nationally due to a lack of awareness among surgeons and a limited ability to evaluate patients for certain peritoneal-based cancers.
“Physicians should be cognizant of [the relationship] at the time of the operation,” Sicklick said. “And if small peritoneal implants are found, to not ignore them but think about removing them for diagnostic and potentially treatment purposes.”
When peritoneal mesothelioma is diagnosed early, it can be treated more effectively using cytoreductive surgery and intraoperative chemotherapy, leading to a survival of five to 10 years and beyond.
Too often, though, it is diagnosed in later stages, leading to less effective mesothelioma treatment, a quicker relapse and much shorter survival.
“In terms of an immediate, direct benefit from these findings, it’s hard to say,” Sicklick said. “At this point, the benefit isn’t in terms of a new drug, but in terms of decision-making.”