NCI Moving Closer to More Effective Treatment for Pleural Mesothelioma
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco
A research team at the National Cancer Institute is developing a novel therapy that could change the treatment paradigm for pleural mesothelioma. It is a long-awaited, much-needed breakthrough.
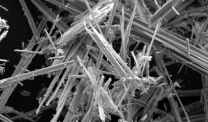
The potential intraoperative adjuvant is a spray-on hydrogel involving genetically engineered molecular nanoparticles designed to specifically target and kill tumor cells.
It showed surprising efficacy in a recent laboratory study at the NCI with mesothelioma models in mice. Nature Nanotechnology published the study, detailing the impressive results.
“This could be a huge deal, potentially a real game-changer in treating this disease,” Dr. Chuong Hoang, thoracic surgeon at the NCI, told The Mesothelioma Center at Asbestos.com. “Yes, I’m excited by what we’ve seen.”
Gel Could Kill Tumor Cells That Evade Surgery
Hoang believes the new therapy could potentially be used alongside surgery to kill the microscopic tumor cells that typically evade detection and later cause the inevitable recurrence of mesothelioma, a cancer with no cure.
Aggressive surgery is still viewed as the most effective treatment for pleural mesothelioma, but less than 20% of those who have it survive more than five years.
“It’s so disappointing that after surgery, inevitably the tumor comes back. You just can’t remove every last bit of it,” Hoang said. “That’s why this could be a game-changer, seen as a molecular knife to finish the job and go after the microscopic stuff that we otherwise couldn’t see. This could make surgery something better than it already is.”
Developing a reliable adjuvant with aggressive surgery for pleural mesothelioma has been ineffective to this point. Photodynamic therapy and intraoperative chemotherapy – similar to what works well with peritoneal mesothelioma in the abdomen – have shown only limited success. Novel immunotherapy as an adjuvant to surgery is in its early stages of development.
Mesothelioma Remains a Unique Challenge
A major reason for the ineffectiveness of adjuvants has been the diffuse nature of mesothelioma cancer, which grows in thin sheets atop normal tissue. This makes it almost impossible to totally remove it with surgery from all the body’s natural crevices.
This slow-release hydrogel, though, can be sprayed onto large complex surfaces and can react to tissue alterations over days and weeks. Unlike chemotherapy, it also can be engineered to target only specific cancer cells and not non-cancerous tissue.
The novel hydrogel was tested with four mouse models by scientists at Hoang’s lab in the Center for Cancer Research, housed in the National Cancer Institute.
A single injection of the hydrogel successfully reduced tumor growth in mice in the NCI’s first model.
In the second model, when the hydrogel was spread over several organs with complex surface topology and allowed to settle for a week, it slowed tumor progression and increased survival time.
Another single injection of the hydrogel in the chest wall and lungs during the third model again reduced disease progression.
With the fourth and final model, the hydrogel was spread following a cancer surgery. After one month, only faint tumor recurrence was seen where it was used, while the untreated areas saw explosive tumor growth.
“Whether or not it will work like it does in mice, we’ll have to see,” Hoang said. “We don’t want to overpromise, jump ahead and fall flat on our face, but based on how the technology works, it’s low toxicity, and even if it fails at the next step, it won’t hurt anyone.”
Thinking Big for the Future
Hoang believes the novel treatment could move into the clinical trial stage within 2-3 years, if everything goes well.
“We’re a few years away yet, taking it from the laboratory to human testing,” he said. “We should demonstrate its viability with larger animals first. But we fully believe we can make it all the way to the end cap.”
He also believes the concept has potential to work with other surface-growing malignancies such as brain tumors and ovarian cancer. He has hopes that eventually it could be used as a first-line treatment for mesothelioma.
“The grand prize would be if we are able to use this method as front-line treatment without having to put people through that giant surgery,” Hoang said. “That would be very special.”