Mesothelioma Clinical Trial to Involve Drug Studied for COVID-19
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco

A novel phase II clinical trial for malignant mesothelioma is expected to open soon and involve a versatile, biological drug already showing promise in treating severe cases of COVID-19.
Oncotelic Therapeutics Inc., an innovative, immunotherapy/oncology company in Agoura Hills, California, hopes to open the mesothelioma clinical trial by March at a dozen prominent U.S. treatment centers, including the Cleveland Clinic Cancer Center, University of Pennsylvania Medicine in Philadelphia and Fred Hutchinson Cancer Research Center in Seattle.
“We’re excited about the potential. There is a huge unmet medical need with mesothelioma. The hope is that we can use this to increase the response to checkpoint inhibitors,” Dr. Anthony Maida, chief clinical officer at Oncotelic, told The Mesothelioma Center at Asbestos.com. “The goal is to help these patients live longer, better lives.”
OT-101 is the name of the biologic, made from complex molecules and manufactured using living microorganisms. It works by inhibiting transforming growth factor beta (TGF-beta), a protein that suppresses a patient’s own immune system and allows tumors to flourish.
TGF-beta is expressed in many cancers, but in particularly high levels with mesothelioma tumors.
“We are essentially trying to suppress the suppressor,” Maida said.
Drug Helps the Immune System Work
Both tumor cells and the coronavirus induce TGF-beta as part of their immune evasion mechanism, potentially making OT-101 impactful with COVID-19 and cancers.
The OT-101 treatment already showed positive activity in a recently completed phase II clinical trial involving patients hospitalized with severe COVID-19 symptoms.
It also will be tested soon with glioblastoma, lung and colorectal cancers, according to Oncotelic Therapeutics.
OT-101 will be used in the upcoming mesothelioma study in combination with checkpoint inhibitor drugs, the most common of which are pembrolizumab and nivolumab, both already being used in various ways to treat mesothelioma.

Try our new clinical trials search tool to find active trials near you. Get help enrolling today.
Find a Clinical TrialImproving Checkpoint Inhibitors
The effectiveness of checkpoint inhibitor drugs with mesothelioma has been inconsistent. It has worked exceptionally well, but only for a small percentage of patients.
“What we’re hoping is that by combining with checkpoint inhibitors, we will see a better response in more patients. We would love to get the 20%-25% effectiveness that there is now to 50% effectiveness,” Maida said. “We can help these patients.”
The FDA recently approved the checkpoint inhibitor combination of nivolumab and ipilimumab, also known by brand names Opdivo and Yervoy, for first-line treatment of pleural mesothelioma.
The median survival improvement for patients, though, was only modest for the most common subtype of disease when compared to standard chemotherapy.
That’s where OT-101 could make a difference if proven effective in early clinical trials.
“The major reason for the failure of these checkpoint inhibitor drugs with mesothelioma is the high levels of [TGF-beta],” Maida said.
OT-101 Trial Will Boost Research Efforts
The upcoming clinical trial will not only test the influence of OT-101 on the checkpoint inhibitors but will be used to help identify more predictive biomarkers for TGF-beta.
CAR T-cell therapy, for example, which involves the modification of a patient’s own T cells, has been shown in the laboratory to benefit greatly from the inhibition of the TGF-beta protein. The long-range hope is to find better ways to counter defense mechanisms used by the tumor cells.
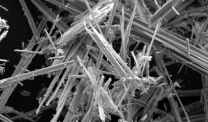
Mesothelioma is a rare cancer with no definitive cure, diagnosed in an estimated 3,000 people within the U.S. annually. It is most often caused by the inhalation of toxic asbestos fibers.
“This is the first of a series of planned clinical trials in patients with various solid tumors evaluating clinical benefit, while also assessing a host of parameters associated with changes in the tumor microenvironment,” Maida said. “We’re moving forward.”