Researchers Study New Immunotherapy Combination for Mesothelioma
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco

The immunotherapy combination of tremelimumab and durvalumab has shown surprising efficacy, particularly as a second-line treatment option for patients with pleural mesothelioma, according to a recent study.
Its effectiveness, comparable to a similar combination which was approved in 2020 by the U.S. Food and Drug Administration, further illustrated the new direction for future treatment of mesothelioma.
Chemotherapy will no longer be the stand-alone, standard-of-care treatment for most patients.
“Promising results have emerged on the use of targeted treatment with immune checkpoint inhibitors (ICI), particularly when given in combination regimens,” the study authors wrote. “The study results further support the efficacy of combined ICI therapy in mesothelioma.”
The Lancet Respiratory Medicine journal published results of the phase II clinical trial conducted by the Department of Oncology at University Hospital in Siena, Italy. Corresponding author Dr. Michele Maio was unavailable to provide his perspective.
Drugs Help Body Target Cancer Cells
The study involved 40 patients who received both tremelimumab and durvalumab intravenously every four weeks for four doses, followed by maintenance durvalumab for nine more weeks.
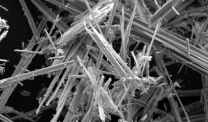
The drugs are known as immune checkpoint inhibitors, a class of immunotherapy drugs that help a patient’s own immune system combat cancer cells.
Durvalumab, also known by the brand name Imfinzi, works by negating the PD-L1 protein that often allows tumor cells to avoid a patient’s immune system.
Tremelimumab complements durvalumab by blocking a receptor on the immune cells that normally stops an immune attack.
At a median follow-up of 52 months, five of the 40 patients were alive. More than a third of the patients achieved a long-lasting objective response.
Results included:
- 65% immune-related disease control
- Median overall survival of 16.5 months
- 20% survival at 36 months
- 15% survival at 48 months
Immunotherapy Retreatment Options Examined
According to the authors, this also was the first study that measured the safety and efficacy of retreatment involving a combination of immune checkpoint inhibitor drugs.
Typically, treatment with immunotherapy drugs in a clinical trial is stopped and not restarted once disease progression is discovered.
Seventeen of the 40 patients were part of the retreatment phase of this study. Patients who had disease progression following partial response or stable disease were eligible for retreatment.
Survival at 12 months after the retreatment was 52.9%, and 23.5% at 24 months. There were no serious immune-related adverse effects among the 17 patients.
“For patients with mesothelioma who have disease progression after an initial clinical benefit, retreatment with these same agents might be a useful option,” the authors wrote.
Seven of the 17 patients in the retreatment cohort achieved immune-related stable disease. For three of those, stable disease lasted at least 11 more months.
The median overall survival of those in the retreatment cohort was 25.6 months, compared to just 11 months for those who received chemotherapy as their second-line treatment.
“First-line combination treatment has been shown to significantly improve overall survival compared with platinum-based therapy for patients with pleural mesothelioma,” the study authors concluded. “And it is likely to become the new standard of care in this setting worldwide.”
Researchers Also Studying Combination Therapy
The same two-drug combination also is being studied at the Baylor College of Medicine in conjunction with aggressive surgery. The ongoing study hopes to determine if durvalumab and tremelimumab, or durvalumab alone, is more effective with surgery.
Thoracic surgeon Dr. Bryan Burt is the lead investigator of the Baylor study.
Durvalumab is part of a phase III international study measuring its effectiveness when used in combination with the chemotherapy drugs pemetrexed and cisplatin. The immunotherapy drug was first approved by the FDA in 2017 for bladder cancer and has shown early effectiveness with certain lung cancers.
Among the U.S. part of the trial are the Seattle Cancer Care Alliance, Stanford Cancer Institute in Palo Alto, California, and Fox Chase Cancer Center in Philadelphia.
While immunotherapy has worked well for some mesothelioma patients, it typically has not been effective for the majority, creating a need to better identify who will benefit before treatment begins.
The authors in Italy believe this latest study could help serve that purpose – identifying tumor mutational burden as a potential marker for immune checkpoint inhibitor drugs.
“A high mutational load at baseline seems to identify patients with mesothelioma who are most likely to benefit from ICI therapy and retreatment with these agents,” the researchers wrote. “This finding is intriguing and needs to be further explored.”
They also believe the use of immunotherapy to treat mesothelioma will grow considerably in coming years. The FDA approved nivolumab and ipilimumab as a combined treatment in 2020, the first new treatment option for mesothelioma in almost two decades.
“Anti-tumor immunotherapy with immune checkpoint blockade in patients with mesothelioma has yet to reach its full potential,” study authors wrote. “Further investigation is warranted for potential application of retreatment in the clinical practice.”