CAR T-Cell Therapy Showing Promise with Pleural Mesothelioma
Research & Clinical TrialsWritten by Tim Povtak | Edited by Walter Pacheco
Memorial Sloan Kettering Cancer Center continues its drive toward a future that may involve innovative CAR T-cell therapy as part of standard-of-care treatment for malignant pleural mesothelioma.
The latest step was a clinical trial exploring a first-in-human, intrapleural-administered CAR T-cell therapy used in combination with pembrolizumab, a well-known immunotherapy drug also known by the brand name Keytruda.
Results were impressive, including a 23.9-month median overall survival and an 83% one-year survival rate for patients. Cancer Discovery published the single-center study results July 15.
“There is more work to be done, but what we saw was very encouraging,” thoracic surgeon and lead study author Dr. Prasad Adusumilli told The Mesothelioma Center at Asbestos.com. “We are moving forward.”
Adusumilli, vice chair for translational research at Memorial Sloan Kettering, predicted years ago that CAR T-cell therapy would one day “change the paradigm of treating mesothelioma.” Nothing since has changed his mind.
CAR T-Cell Therapy Helped by Pembrolizumab
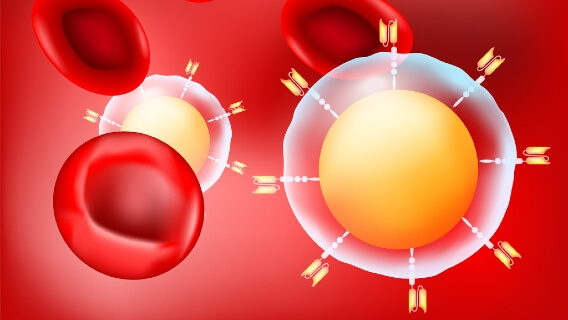
CAR T-cell therapy, also known as chimeric antigen receptor T-cell therapy, involves the laboratory reprogramming of a patient’s T cells, white blood cells that discourage infection and disease. In the laboratory, the cells are genetically modified to better recognize and fight the cancer.
In the past, T-cell therapies have been effective only when treating blood cancers such as lymphoma and leukemia, but not with solid tumors such as pleural mesothelioma, a rare cancer with no cure.
The biggest problem has been the therapy’s lack of durability and endurance, along with an inability to infiltrate the tumors. Memorial Sloan Kettering has been at the forefront of trying to change that.
This recent study cited three factors that led to success in the trial, and made it a first-in-humans study:
- CAR T-cell therapy was reprogrammed to target mesothelin, a cell surface protein that lines the pleura and pericardium and is overexpressed in several different cancers, including mesothelioma.
- The therapy was regionally administered, either through a pleural catheter or via interventional radiology-guided imaging.
- CAR T-cell therapy was followed by individual doses of pembrolizumab, which serves to block the interaction of PD-1, a protein that often prevents a patient’s immune system from attacking the cancer.
Almost all patients received cyclophosphamide, a preconditioning chemotherapy, two to seven days before receiving the CAR T-cell infusion.
The median time from white blood cell removal until therapy infusion was 3.2 months.

Try our new clinical trials search tool to find active trials near you. Get help enrolling today.
Find a Clinical TrialSurvival Results Are Encouraging
In the study, 23 patients receiving only the cyclophosphamide and the CAR T-cell therapy managed a median survival of 17.7 months from time of infusion and a 74% one-year survival.
The 18 patients who also received the pembrolizumab managed a 23.9-month median survival and an 83% one-year survival. Eight of those patients sustained stable disease for at least six months.
By comparison, the immunotherapy combination of Opdivo and Yervoy managed a median overall survival of 18.1 months in a phase III clinical trial, leading the U.S. Food and Drug Administration to approve the treatment in 2020. It was the first new drug regimen approved for mesothelioma in 16 years.
Patients receiving only standard-of-care chemotherapy – which is the most common treatment today for those with unresectable disease – typically live for less than 12 months.
In this recent study, a 76-year-old patient saw a 28% reduction in tumor lesions with the CAR T-cell therapy and a 78% reduction after the follow-up pembrolizumab treatment. His response lasted for 26 months.
Another patient receiving both the CAR T-cell therapy and pembrolizumab had no measurable disease for 32 months. A third patient was found to have a 40% tumor reduction at 16 months.
Next MSK Clinical Trial Now Enrolling
Researchers noted in their study that the combination treatment – and the synergy sparked – consistently showed an improved CAR T-cell persistence, more effective destruction of cancer cells and decreased cell exhaustion.
“You must keep in mind, this was a phase I trial. We can’t get ahead of ourselves,” Adusumilli said. “There still are more steps to be taken, but we are optimistic that we can translate success to patients in the coming years.”
Memorial Sloan Kettering already has begun recruiting and treating patients for its next clinical trial involving CAR T-cell therapy and mesothelioma.
In this latest, dose-escalation trial, the anti-PD-1 agent pembrolizumab will be woven into the T-cell therapy instead of being administered as a follow-up.
This trial is expected to run until 2023.







