Phase III Trial of Durvalumab for Mesothelioma Underway
The U.S. Food and Drug Administration will be closely watching the latest, international phase III clinical trial for unresectable pleural mesothelioma involving the immunotherapy drug durvalumab.
FDA approval may be coming soon.
“It looks very promising,” Dr. Arkadiusz Dudek, of Regions Hospital Cancer Care Center in St. Paul, Minnesota, told The Mesothelioma Center at Asbestos.com. “The hope is to have the regimen approved by the FDA as front-line therapy. There is a real need today for more options with mesothelioma.”
The goal of the randomized trial – officially known as DREAM3R – is to determine how much overall survival improves by combining durvalumab with standard chemotherapy of pemetrexed and cisplatin.
Dudek is a principal investigator for the Metro-Minnesota Community Oncology Research Consortium, one of the first four U.S. locations that began accepting patients in March.
The other centers are Johns Hopkins Sidney Kimmel Cancer Center in Baltimore, the Cleveland Clinic in Ohio and the University of Michigan in Ann Arbor. Several more are expected to join soon. The start of the trial was delayed at several sites because of the COVID-19 pandemic.
Patients throughout New Zealand and Australia are also being recruited.
“There is potential of this becoming part of a new standard of care for mesothelioma,” Dudek said. “It is exciting to have this study going on. This is where treatment improvements are made.”
Durvalumab Could Fill Mesothelioma Treatment Void
In 2020, the FDA approved the immunotherapy combination of Opdivo and Yervoy, known generically as nivolumab and ipilimumab, for the treatment of mesothelioma. It was the first new systemic treatment in 15 years.
While the combination more than doubled survival time for the toughest-to-treat mesothelioma cell types – sarcomatoid and biphasic – in a phase III trial, the improvement was much more modest for epithelioid mesothelioma, the most common type.
Dudek and others believe that durvalumab could fill that void for those with epithelioid mesothelioma.
“We expect that the DREAM3R trial will be a particularly good treatment option for the 75% of mesothelioma patients with epithelioid subtype,” said Dr. Patrick Forde, director of the Thoracic Cancer Clinical Research Program at Johns Hopkins Medicine and lead investigator for the U.S. portion of the trial. “We have seen particular benefit in the epithelioid population from the chemo-durvalumab combination.”
Drug Found Effective in Phase II Clinical Trials
This latest study was sparked by significant effectiveness in two independent phase II trials, in the U.S. and in the Australia/New Zealand region.
The earlier U.S. trial reported median overall survival rates of 70.4% and 44.2% at 12 and 24 months, respectively, for all subtypes combined.
Median overall survival was 20.4 months, almost double the historical control of 12.1 months with only standard chemotherapy.
The Australia/New Zealand study reported that 31 of its 54 patients reached the six-month progression-free survival stage.
Investigators with the DREAM3R study hope to enroll 480 patients with unresectable pleural mesothelioma. They will be randomized 2:1 to receive durvalumab plus four to six cycles of chemotherapy, or chemotherapy alone.
Patients in the experimental group will continue with maintenance durvalumab until unacceptable toxicity, disease progression or patient withdrawal. Patients receiving only the chemotherapy option will be offered second-line treatment upon disease progression.
Immunotherapy Is Expanding Its Reach
AstraZeneca, a multinational biopharmaceutical company, produces and markets durvalumab under the brand name of Imfinzi.
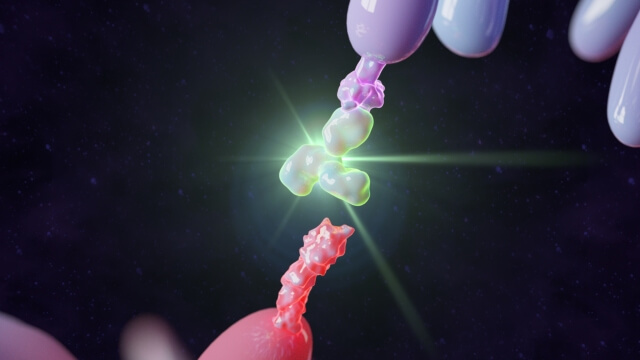
Durvalumab produces an antibody known as a checkpoint inhibitor, negating the protein protecting the cancer cells from a patient’s own immune system. It allows the immune system to more easily identify and kill the cancer cells.
The drug was approved by the FDA for bladder cancer in 2017 and has shown considerable effectiveness with certain types of lung cancer.
It also is part of eight different mesothelioma clinical trials in various stages and in various combinations. Baylor College of Medicine in Houston has been studying its effectiveness in combination with surgery.
The Dana-Farber Cancer Institute in Boston is studying durvalumab for second-line treatment with tremelimumab, another immunotherapy drug.
“This is an exciting time for the intersection of immunotherapy and mesothelioma,” Dudek said. “It is a very promising time with lots of hope for long-term disease control that lasts for many months, if not many years.”