Thoracic Chemotherapy May Advance Mesothelioma Treatment
Thoracic surgeon Dr. Marcello Migliore is convinced that adding hyperthermic intrathoracic chemotherapy to aggressive surgery can extend survival significantly for patients with pleural mesothelioma cancer.
He wants others to know that, too.
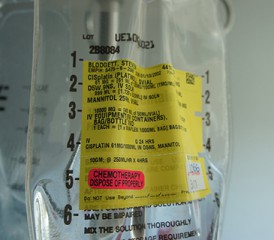
This seldom-used, controversial procedure, also known as HITHOC, involves circulating a heated, high-concentration chemotherapy solution throughout the chest cavity for 60 minutes immediately following aggressive mesothelioma surgery.
The idea is to kill any microscopic tumor cells that evaded the surgeon, hopefully slowing a potential cancer recurrence.
Unlike HIPEC, a similar procedure used effectively for peritoneal mesothelioma in the abdominal cavity, HITHOC’s benefits have not been fully proven in a large-number, well-controlled clinical trial. So doubters remain.
“I have personally seen very good results with it, some unbelievable results with it,” Migliore, renowned thoracic surgeon at University of Catania in Italy and University Hospital of Wales, told The Mesothelioma Center at Asbestos.com.
“We still need a global trial to prove its worth,” he said. “But more surgeons should be using it now. I want to see more patients benefiting from it.”
Doctor Urges Addition to Mesothelioma Guidelines
Migliore wrote an editorial last month in Annals of Translational Medicine, questioning why the use of HITHOC for pleural mesothelioma is not in the treatment guidelines of reputable publications.
Neither the National Comprehensive Cancer Network nor the American Society of Clinical Oncology guidelines include it for treatment of pleural mesothelioma, much to his frustration.
Early in 2021, Migliore will be publishing a paper detailing some of his most recent successes using HITHOC in combination with pleurectomy and decortication surgery.
“This needs to be known by as many patients as possible, as many surgeons as possible, to give more hope to those with pleural mesothelioma,” he said. “We’re not going to cure this disease, but we are going to give these patients a longer survival with this treatment.”
Some Question HITHOC Benefits for Pleural Mesothelioma
Mesothelioma specialists have been experimenting with the HITHOC procedure, with varied results, for more than a decade.
Mesothelioma pioneer and thoracic surgeon Dr. David Sugarbaker led a retrospective study published in 2013 that showed a 35.3-month median survival for patients undergoing HITHOC, compared to a 22.8-month survival for surgical patients going without HITHOC.
The majority of those patients, though, underwent an extrapleural pneumonectomy, an even more aggressive surgery rarely done today.
Most recent studies involving HITHOC have focused on the safety and feasibility of the procedure in the context of complete surgical resection. Less than a third of patients diagnosed with pleural mesothelioma even qualify for aggressive surgery.
Migliore led the most recent study, comparing surgery with HITHOC to surgery with talc pleurodesis for mesothelioma patients treated in Catania, Italy.
The European Respiratory Journal released the study abstract in October 2020.
Thirteen patients receiving HITHOC with surgery had a median overall survival of 33 months, compared to just 19.6 months for the 14 patients not getting HITHOC.
One- and two-year survival rates were 69% and 54% respectively for those getting HITHOC, compared to 57% and 28.6% for those not getting HITHOC.
Large Mesothelioma Clinical Trial Needed
The reluctance in using the procedure – even at high-volume specialty centers – stems from the absence of a controlled clinical trial, often a problem with rare diseases and even rarer procedures.
There is no standardized therapy protocol concerning precise technique and discrepancies in the methods for the use of HITHOC. Severe complications, including complete renal failure, have been reported.
“It is demanding technically and prolongs surgery significantly,” Dr. Loic Lang-Lazdunski, thoracic surgeon and mesothelioma specialist at Quebec Heart and Lung Institute at Laval University, told The Mesothelioma Center at Asbestos.com.
“I’ve not seen a survival benefit in controlled trials,” he said. “This is a different beast than peritoneal mesothelioma. I cannot really see a point in using this method in pleural mesothelioma, a chemo-resistant tumor.”
Lang-Lazdunski has had great success combining his aggressive surgery with a pleural lavage of antiseptic povidone-iodine, along with radiotherapy and systemic chemotherapy.
Multimodal therapy has typically been the gold standard for extending survival with pleural mesothelioma. It involves a combination of aggressive surgery, local radiation and systemic chemotherapy.
By using HITHOC directly in the chest cavity – and not intravenously as used in standard practice – the chemotherapy can be heated and more concentrated, better able to kill tumor cells.
“Yes, I’ve been surprised that more of the big centers are not using this procedure today,” Migliore said. “The guidelines in place today have demonstrated that most treatments for mesothelioma are weak. We can, and should, do better.”