Mesothelioma Trial to Test Cancer Vaccine with Immunotherapy
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco

A research team at Oslo University Hospital in Norway has opened a mesothelioma clinical trial using the novel UV1 cancer vaccine alongside a promising immunotherapy combination.
UV1 is a peptide-based vaccine designed to induce a specific T-cell response and increase the effectiveness of the immunotherapy drugs.
This is the first time UV1 will be studied with mesothelioma cancer, but it already has shown safety and signs of efficacy when used on malignant melanoma, prostate cancer and lung cancer in studies worldwide.
It will be used with the immunotherapy combination of nivolumab and ipilimumab, also known by brand names Opdivo and Yervoy, respectively.
UV1 is a product of Ultimovacs, a pharmaceutical company based in Oslo, Norway. The study will soon move into six other national hospitals, covering Sweden, Spain, Denmark and Australia.
“Even if we can’t promise efficacy at this point, we believe mesothelioma is a relevant cancer in which to test this vaccine,” Dr. Jens Bjorheim, chief medical officer at Ultimovacs, told The Mesothelioma Center at Asbestos.com. “The hope is clinical efficacy and overall survival benefit.”
Pleural Mesothelioma Patients Part of Trial
The phase II, randomized study involves treatment in a second-line setting after tumor progression with first-line chemotherapy for those with unresectable disease.
Bristol Myers Squibb, the pharmaceutical giant producing the immunotherapy combination, is one of the study collaborators.
The first patient was dosed on June 15. The study is expected to report on the efficacy endpoint in 2022 and includes 118 patients with pleural mesothelioma. Half will receive just nivolumab and ipilimumab — known as checkpoint inhibitors — and the other half additionally will be treated with the cancer vaccine.
Researchers believe there is a synergistic effect when the vaccine is used with the checkpoint inhibitors.
UV1 works by targeting telomerase, a cancer antigen that helps cancer cells divide uncontrolled. By targeting telomerase, the immune system can better recognize the cancer cells and destroy them.
“The vaccine helps the immune system do its job,” Bjorheim said. “Hopefully, the vaccine further enhances what the immune system is designed to do — kill cancer cells.”
The immunotherapy combination of nivolumab and ipilimumab already has shown promise in earlier trials with pleural mesothelioma.
At the World Conference on Lung Cancer annual meeting in August, authors of one first-line immunotherapy study showed increased survival for mesothelioma patients when comparing the nivolumab/ipilimumab combination to standard chemotherapy.
Although the median overall survival advantage was modest — 18.1 months compared to 14.1 months — it was more dramatic for those with the traditionally tougher-to-treat mesothelioma subtypes.
For patients with non-epithelioid histology, median survival was only 8.8 months with standard chemotherapy, but 18.1 months for those receiving the immunotherapy combination. The overall survival rate was 38% for the immunotherapy group, and only 8% for the chemotherapy group.
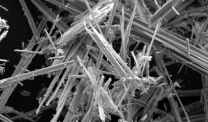
Mesothelioma is an aggressive cancer most often caused by long-ago exposure to asbestos. There is no definitive cure for mesothelioma, despite recent treatment advances. It is diagnosed in an estimated 3,000 people annually in the U.S. About 20% of those diagnosed with pleural mesothelioma — which begins in the thin lining around the lungs — live three years after diagnosis.
Immunotherapy Is Future of Mesothelioma Care
Like most in the medical community, Bjorheim believes the future of cancer care involves the use of immunotherapy. Finding the right combinations, though, has been difficult, especially for rare cancers such as mesothelioma.
UV1 was part of another clinical trial involving malignant melanoma and combined with pembrolizumab, also known as Keytruda, a different checkpoint inhibitor drug.
“There are a huge number of combinations out there being tested today,” Bjorheim said. “Some are different types of immunotherapy, and some are immunotherapy combined with older-type treatments. Immune therapy, in a way, has revolutionized cancer care in the last decade.”