Mesothelioma T-Cell Therapy Shows Early Effectiveness in Trial
A mesothelioma clinical trial involving genetically modified T cells has opened to considerable acclaim, shrinking tumors in the first five patients who were treated.
The phase I portion of the clinical trial is designed to define the safety profile and optimal dosage level of TC-210, a novel immunotherapy targeting mesothelin, a cell-surface protein often overexpressed in several cancers.
While T cell modifications in the laboratory are proving safe and well tolerated, the initial signs of consistent efficacy became an early bonus in phase I.
Four of the patients treated had mesothelioma. The fifth had ovarian cancer. All five had previously undergone treatment that failed, including one targeting mesothelin.
Two of the five patients already had registered for hospice care before backtracking into the clinical trial.
“What we’ve seen in the first few patients is very encouraging,” Dr. Alfonso Quintás-Cardama, chief medical officer at TCR2 Therapeutics, which is sponsoring the trial, told The Mesothelioma Center at Asbestos.com. “We’ve seen consistent benefits across the board. This early data is quite meaningful.”
Major Cancer Centers Hosting T-Cell Trial
The study, which soon will move into phase II, is being conducted at five top cancer centers across the country. They are:
“It’s very early yet, but my hope is that what we’ve seen so far can be replicated in subsequent patients,” Quintás-Cardama said. “I know people are paying all this attention to the efficacy we’ve seen, but the focus now is still on safety.”
All five patients in the trial showed tumor regression with TC-210, including two with partial responses and two with stable disease through six months. The disease control rate among the five was 100%.
“We could not be happier with our start of this clinical trial,” Garry Menzel, president and chief executive officer at TCR2 Therapeutics, said during a recent presentation to investors. “We are motivated by the desire to bring a truly novel therapy that can have a transformational impact for cancer patients.”
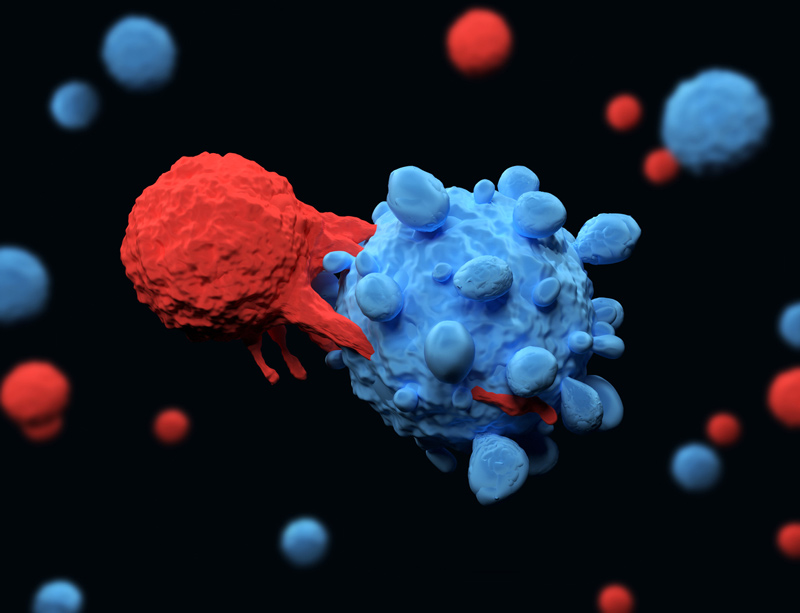
T-Cell Therapy for Mesothelioma
The early success of this clinical trial has been especially notable because, until recently, T-cell therapy had not shown effectiveness with advanced-stage solid tumors, such as mesothelioma. Its success had been with blood cancers such as leukemia and lymphoma.
The U.S. Food and Drug Administration approved the first T-cell therapy for pediatric leukemia in 2017.
“The early TC-210 data suggests our approach may overcome the challenges faced by many T-cell therapies in the hostile solid-tumor microenvironment,” Quintás-Cardama said.
T-cell therapy is based upon a patient’s unique genetic profile and a modification of their T cells, a type of white blood cell that is separated from the blood through a process known as leukapheresis.
This process can take up to four weeks before the T cells are reintroduced with an ability to identify and potentially eliminate tumor cells by targeting mesothelin.
“It’s like an engine with many different parts. Most of the T-cell therapies employ only one or two of those parts,” Quintás-Cardama said. “We engage all of them. That makes a difference. It’s much more complex, much more difficult to do.”
T-Cell Clinical Trial Moving Soon to Phase II
The current clinical trial is also open to certain types of non-small cell lung cancer, ovarian cancer and cholangiocarcinoma. Individual levels of mesothelin expression must be satisfied to be eligible for the trial.
More patients beyond the first five already are enrolled and are being treated. Phase I patients are receiving a one-time infusion and are actively followed for six months.
Once a dosage level has been established phase II will begin, with each patient receiving first a preconditioning chemotherapy drug and then TC-210. A small number of patients also will be getting pembrolizumab (Keytruda), another immunotherapy drug with a different target, to look for possible synergy with TC-210.
A second infusion is possible if ordered by the study physician. For up to two years, patients will be asked to return regularly to the clinic. Blood samples will be taken approximately 30 times throughout the 24-month period.
“It’s a complex, complicated, laborious therapy, a completely new way of attacking these tumors,” Quintás-Cardama said. “We’re genetically reprograming a patient’s immune system to attack their cancer. And we’re seeing success.”
TCR2 Therapeutics is a clinical-stage immunotherapy company based in Cambridge, Massachusetts, and focused on developing T-cell therapies for solid tumors and hematological malignancies.