UPenn Research with Mesothelioma Blood Test Shows Promise
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco

Scientist Ian Blair at the University of Pennsylvania School of Medicine believes his team is close to identifying the variant of a blood-based biomarker that could diagnose asbestos disease in its earliest stages.
If successful, it could clear the path to a more treatable — and potentially curable — stage of malignant mesothelioma cancer.
“This could be a big deal. We’re trying to become the first,” Blair told The Mesothelioma Center at Asbestos.com. “We hope to have it within the year.”
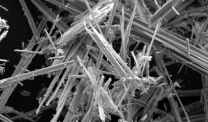
The potential breakthrough involves the HMGB1 (High-Mobility Group Box 1) chromosomal protein and its variants, which can be secreted through different pathways.
Mesothelioma tumor cells secrete a form of HMGB1, which promotes an inflammatory condition and the proliferation of tumor cells.
Blair’s team has developed and validated a laboratory procedure to quantify HMGB1 in plasma through high-resolution mass spectrometry.
Identifying Asbestos-Related Biomarkers
The key is identifying the protein variation exclusive to asbestos-related diseases such as mesothelioma. HMGB1 can be found in numerous diseases, some less serious than this aggressive cancer.
“Two things you want: 100% specificity, so you only detect people with this disease; and 100% sensitivity, so you can detect everyone with this disease,” Blair said. “Right now, I’m very encouraged. We’re working extremely hard on this. The mood is pretty upbeat.”
Blair and his team have been working on the project involving asbestos exposure for almost five years. He is an investigator for the Abramson Cancer Center at the University of Pennsylvania School of Medicine, one of the country’s leaders in cancer research.
His expertise involves the use of molecular biology and mass spectrometry as tools for discovering biomarkers in early detection of rare cancers.
Early Mesothelioma Diagnosis Is Key
The concept of an earlier diagnosis is critical to advancing treatment for mesothelioma, a disease with a poor prognosis and no cure. It typically is not diagnosed until its latter stages, when treatments are limited.
“It’s usually too late to do anything effective, but that’s what drives me today, because that’s the holy grail of a biomarker,” Blair said. “The mantra is that early detection of most cancers leads to improving outcomes.”
Earlier detection of mesothelioma brings no assurance that survival will be extended — unless it is accompanied by treatment advances.
“Like biomarkers for Alzheimer’s disease, what’s the point of knowing you have it if there is no cure for it?” Blair said. “You could argue the same for mesothelioma. We’re only hoping that early treatment can lead to better results, but there is no magic bullet at this point. Until we develop this, we’ll never know.”
Simple Testing Would Bring Peace of Mind
The diagnostics process for mesothelioma today is often slow and invasive, requiring numerous tests and a biopsy. Even then, it can be elusive and misleading.
A simple blood test like this would allow for the routine testing of high-risk patients with occupational exposure long before any symptoms were present.
Blair’s office has gotten numerous inquiries about his work from those in the Philadelphia public school system, which has been closing and renovating older buildings that were filled with asbestos materials.
He is working with former employees of a nearby factory that was loaded with asbestos products, using their blood samples to help develop the test.
“Imagine the peace of mind in showing people there that they weren’t exposed to asbestos. They could be monitored regularly if we had a test specifically for mesothelioma,” he said.
The quest for better diagnostics with biomarkers for asbestos disease has attracted researchers from around the world.
A biotechnology company in Ontario, Canada, recently unveiled a similar platform that uses mesothelial precursor cells and DNA to predict asbestos disease.
Researchers in Germany have been touting their study of another blood-based protein that is overexpressed in mesothelioma tumor cells and detected through different technology.
“Hopefully, within the year, we’ll have accomplished what we set out to do,” Blair said. “And that will be good.”