Quality of Life Still Good with HIPEC Surgery for Peritoneal Mesothelioma
Research & Clinical TrialsWritten by Tim Povtak | Edited by Walter Pacheco
Surgical oncologist Dr. Edward Levine was not surprised by the encouraging results of the recent study measuring quality-of-life issues following aggressive treatment for patients with peritoneal mesothelioma.
He has been seeing it regularly for several years.
“It just confirmed my clinical gestalt of how patients
did,” Levine told The Mesothelioma Center at Asbestos.com. “But it was nice to now quantify it with standardized, accepted quality-of-life measures.”
The potential benefits outweighed the risks.
Levine, chief of the surgical oncology program at Wake Forest Baptist Comprehensive Cancer Center, is a nationally recognized specialist in peritoneal surface malignancies.
He is the senior author of the study that questioned 46 mesothelioma patients who underwent cytoreductive surgery and hyperthermic intraperitoneal chemotherapy, also known as HIPEC.
Annals of Surgical Oncology published the study in May 2019.
Patients completed surveys preoperatively to establish a baseline, then again at three, six, 12 and 24 months after completion of the surgery and HIPEC combination.
“Patients who go through the treatment tend to have good quality of life after recovering from the acute effects of surgery,” Levine said. “If we can get patients to these procedures, many of them will be long-term survivors.”
Procedure Produces Long-Term Survivors
Much of the work was presented at the Society of Surgical Oncology meeting in Chicago last spring.
Median survival was 3.4 years. One-, three- and five-year survival rates were 77.4%, 55.2% and 36.5%, respectively.
An earlier study at Wake Forest reported a five-year survival rate of 45%, but it included only patients who achieved a complete cytoreduction.
Several patients in this latest study had incomplete cytoreduction with only palliative intent.
The quality-of-life measurements — mental and physical — were considerably higher for those with the complete resection.
Researchers used multiple verified quality-of-life surveys. The median age of the patients was 52.8 years at time of treatment, and 52% were male.

Get the latest tips in this free webinar hosted by top mesothelioma experts.
Get the RecordingMental and Physical Quality of Life
Patients were questioned on topics such as:
- Physical functioning
- Bodily pain
- General Health
- Vitality
- Social functioning
- Mental health
- Depression
Researchers concluded that after treatment, quality of life typically went down before it went up.
When compared to pretreatment measurements, physical function decreased at three months, reached baseline by six months and steadily improved until 24 months.
The emotional well-being scores also were decreased at three months, but significantly increased through the next 21 months.
Authors wrote that the initial decrease in quality of life after surgery likely was because of pain and limitations associated with the large incision and physiologic impact of complications.
They also noted 30% of patients had no significant complications after surgery.
A decrease in quality-of-life measures after 24 months was attributed to disease recurrence.
Procedure Has Become Standard of Care
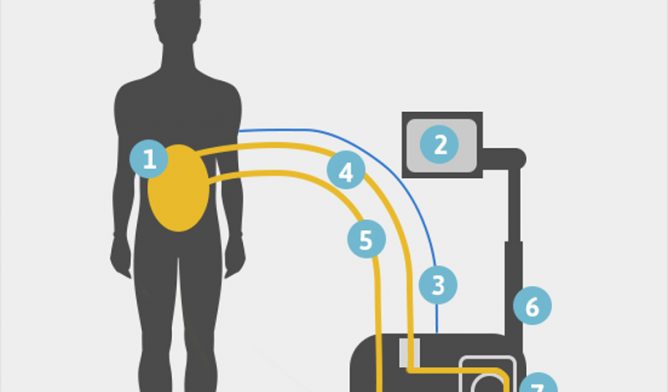
The combination of cytoreduction and HIPEC can be a debilitating procedure, lasting from 8-12 hours.
The surgeon first removes all visible tumor growth, which often has metastasized throughout the abdominal cavity.
A heated chemotherapy solution is then circulated for up to 90 minutes before it is removed.
The high-dose chemotherapy solution is designed to reach the microscopic tumor cells that evaded the surgeon.
The Peritoneal Surface Oncology Group International began listing the treatment combination as standard of care for peritoneal mesothelioma more than a decade ago.
“This is probably the procedure of choice for patients who are candidates for it,” Levine said. “But it is a major operative undertaking with significant risks.”
Procedure Not for Every Patient
With many patients, the disease is too advanced when first diagnosed that it prevents them from being candidates for this aggressive treatment combination.
For those who qualify, though, aggressive treatment most often proves to be worth the risk.
“This study shows that the improvement in quality of life can be very significant compared with the preoperative status,” Levine said. “By six months, virtually all of the patients had recovered to preoperative baseline or better quality-of-life measures.”







