
Sean Marchese is a registered nurse with experience developing and managing respiratory oncology clinical trials and treatments. He has more than 10 years of clinical experience as a nurse in pain management, neurosurgery and clinical trials.

Written by Sean Marchese | Edited by Amy Edel
Mesothelioma presents unique challenges for health care providers. This rare malignant asbestos-related disease affects the lining of the lungs and abdomen. To best treat mesothelioma patients, nursing and medical students should understand all aspects of this aggressive cancer.

Mesothelioma is a type of asbestos-related cancer that forms in the thin, protective tissue covering the lungs, abdominal cavity, heart and testes. Nurses treating these patients should know what causes mesothelioma, why it can be so severe and what they can do to better help this population.
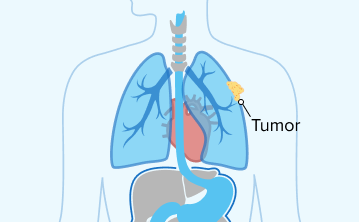
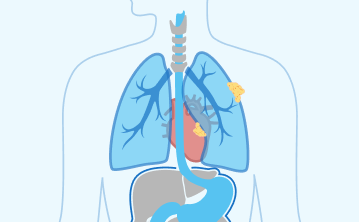
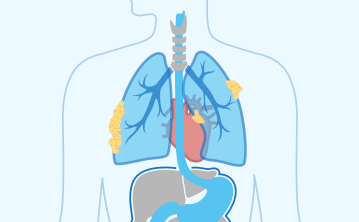
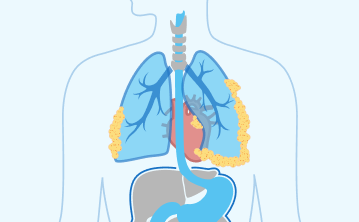
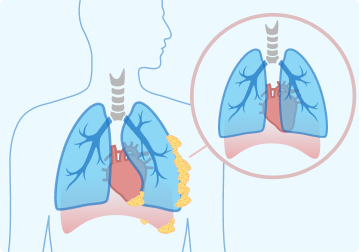
Asbestos exposure is the primary cause of mesothelioma, which can take decades to develop. When tumors form in or on the pleura, the outer lung lining, it’s known as pleural mesothelioma. The pleural form of the cancer accounts for more than 80% of cases in the U.S.
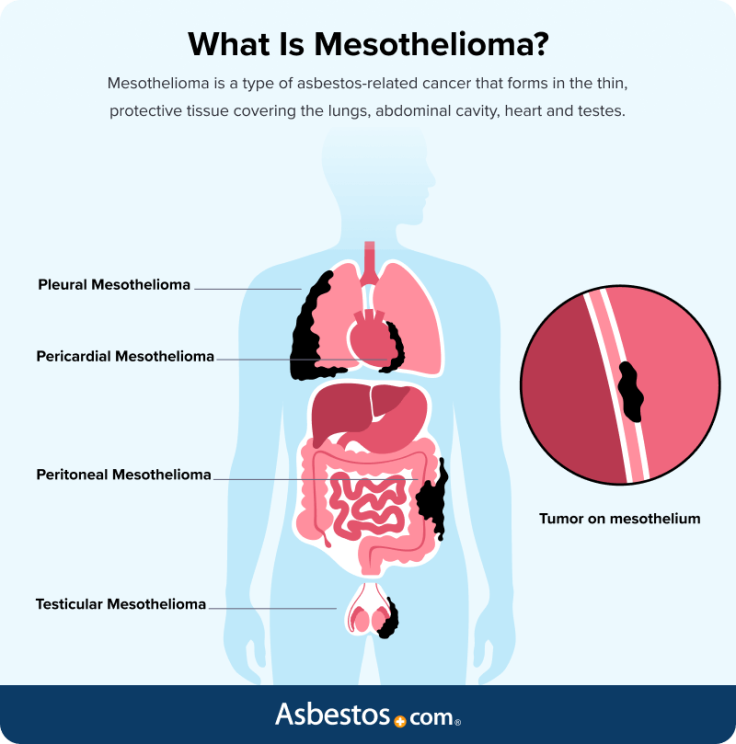
The peritoneum is the protective lining surrounding the organs in the abdomen and connecting them to the abdominal wall. Peritoneal mesothelioma accounts for about 10% to 17% of cases. Symptoms can vary depending on where mesothelioma forms in the body, making diagnosis and treatment difficult.
Even after 40-plus years as a nurse, I knew as much about mesothelioma as the average person — which wasn’t much. Sept. 26 marks Mesothelioma Awareness Day, something I didn’t know existed until I became an advocate for others. That alone shows how much work needs to be done.

Like other cancers, mesothelioma may be malignant and invade other tissues or benign, which is significantly less dangerous. Mesothelioma is multifocal and becomes diffuse as it progresses, often initially forming multiple small tumors in one area and then spreading throughout the body in later stages of the disease.
These grape-like bundles have thin walls and contain a viscous gelatin-like fluid. A biopsy is the only way to determine if mesothelioma is malignant or benign. As a nurse, it’s important to detail and distinguish these differences for patients and outline next steps for either outcome with compassion and care.
| Tumor Characteristics | Benign | Malignant |
|---|---|---|
| Invades Surrounding Tissues and Organs | No | Yes |
| Metastasizes to other parts of the body | No | Yes |
| Irregular cell borders | No | Yes |
| Always requires treatment | No | Yes |
| Can grow to a large size | Yes | Yes |
| Can reoccur | Yes | Yes |
Malignant mesothelioma is more likely to occur 20 to 60 years after asbestos exposure. Benign mesothelioma tumors can occur at any age. Although less dangerous, benign tumors can still cause damage, growing and putting pressure on sensitive organs such as the lungs, heart or kidneys.
Asbestos: A group of 6 naturally occurring minerals known to cause mesothelioma, lung cancer and chronic respiratory illness.
Latency Period: The time between initial asbestos exposure and onset of mesothelioma symptoms, ranging from 20 to 60 years.
Multimodal Treatment: A comprehensive approach to mesothelioma care involving surgery, chemotherapy, immunotherapy and radiation therapy with a multidisciplinary team.
Pleural Mesothelioma: The most common mesothelioma type, affecting the lining of the lungs (pleura). Symptoms include chest pain, shortness of breath and persistent cough. Early detection is vital for differentiating it from other respiratory conditions.
Our writers and experts’ recent research considers all mesotheliomas malignant. Researchers now classify benign growths as well-differentiated papillary mesothelioma tumors. The prefix “malignant” no longer needs to be used to separate mesotheliomas from WDPMT.
Patients are surprised by the way we explain the disease and treatments for them. They’re able to better understand their disease compared to the 5 minutes their doctor had to explain it. Patients really appreciate the wealth of knowledge we provide them. After speaking with us, they feel a lot better about things.

Asbestos exposure is the primary cause of mesothelioma. When you inhale or ingest asbestos fibers, they can become lodged in the lining of the lungs, abdomen, heart or testes, causing inflammation and scarring. These cellular changes damage DNA over time and eventually lead to the development of mesothelioma.
Health care providers, including nurses and medical residents, play a critical role in discussing the causes of mesothelioma with patients. Providing clear, compassionate explanations about how asbestos exposure leads to mesothelioma can help patients understand their diagnosis.

Mesothelioma’s delayed onset underscores the importance of thorough patient histories and a detailed exposure history can play an important role in guiding a patient’s treatment plan. However, patients may have been exposed to asbestos decades ago and may not immediately connect their symptoms to past contact.
The heat-resistant properties of asbestos fibers made them popular for use in construction, industrial applications and the military. Asbestos was also widely used in consumer products such as appliances and textiles.
As a nursing student, recognizing the signs and symptoms of mesothelioma in your patients is crucial for early detection and treatment. Mesothelioma symptoms often mimic those of less severe conditions, which can lead to delayed diagnosis.
According to our research published in The Mesothelioma Center’s State of Meso 2025 survey, patients report fatigue as their most frequent symptom. Listening carefully to your patients and asking targeted questions is essential to uncover potential signs of this rare cancer.
When interacting with your patients, it’s essential to ask if they’ve been experiencing these symptoms, especially if they have a known history of asbestos exposure. For instance, “Have you had any persistent chest pain or difficulty breathing lately?” or “Have you noticed any unusual swelling or unexplained weight loss?” These specific inquiries can help guide you to a more accurate assessment and prompt further investigation.
Early detection of mesothelioma symptoms is critical for improving patient outcomes. Be thorough in your patient assessments. Your vigilance can lead to early diagnosis and treatment of this aggressive cancer.
I think overall our knowledge base regarding any topic related to mesothelioma surprises patients. Our team is seasoned. We all have many, many years of experience, and I believe it shows during the very first call with a patient or caregiver and throughout our relationship.

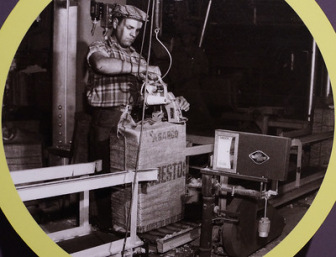
Occupational asbestos exposure is the leading cause of mesothelioma. In the course of workers’ tasks, asbestos fibers could become airborne. Workers inhaled these fibers that then became lodged in their lungs or abdomen, causing long-term damage.
Those working in manufacturing, chemical and power plants often encountered asbestos insulation and other materials. Regular exposure to such environments significantly increases the risk of developing mesothelioma.
Veterans, particularly those who served in the Navy, are at a high risk of developing mesothelioma. Asbestos was extensively used in shipbuilding and other military applications. Many veterans were exposed to asbestos fibers during their service, and this exposure has led to a significant number of mesothelioma cases among them.
Construction workers frequently handle asbestos-containing materials such as insulation, drywall and cement. Firefighters are another group at high risk. Fire damage to buildings can release asbestos fibers into the air, and firefighters can inhale these fibers while performing their duties.
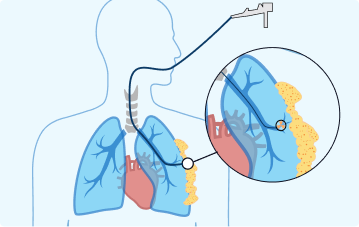
Diagnosing mesothelioma involves a combination of physical exams, imaging tests and biopsies with a thorough review of the pathology report. The cancer’s rarity and nonspecific symptoms can make the diagnostic process challenging.
Early and accurate diagnosis is crucial for effective treatment. Some early tests, such as a fluid test from a pleural effusion, may not test positive for mesothelioma.
Because imaging results don’t conclusively detect mesothelioma, a tissue biopsy is needed for an accurate diagnosis. Helping patients understand their pathology report is crucial, as it provides a clearer picture of their diagnosis and guides treatment decisions.
As a nurse, guiding patients through the diagnostic process with clarity and empathy is essential. Health care providers must ensure patients understand each step along the process as they navigate their diagnoses.
Symptoms of mesothelioma are nonspecific and often resemble those of more common conditions such as the flu, pneumonia or cardiac issues. Many patients initially present with symptoms such as chest pain or shortness of breath, which can delay a correct diagnosis.
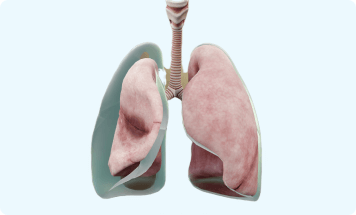
Similar to the advanced forms of these other illnesses, asbestos exposure can also cause pleural effusion and fibroids. Understanding these differential diagnoses is crucial for health care providers to ensure an accurate and timely diagnosis.
Similarities: Adenocarcinoma of the lung and mesothelioma can present with similar symptoms, such as chest pain, coughing and weight loss.
Differences: Adenocarcinoma is a type of lung cancer often related to smoking and other factors. Mesothelioma affects the lining of the lungs or abdomen and is related to asbestos.
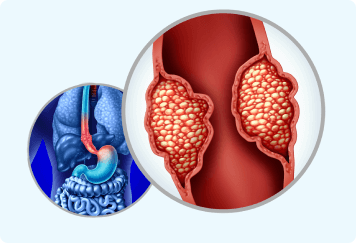
Similarities: In rare cases, peritoneal mesothelioma can be mistaken for the abdominal pain and a diffuse presentation of fibroids.
Differences: Fibroids are benign tumors of the uterus, whereas peritoneal mesothelioma involves malignant cells in the abdominal lining and is related to asbestos exposure.
Similarities: Both conditions can cause scarring and thickening of lung tissues, leading to breathing difficulties.
Differences: Pulmonary fibrosis is typically a result of long-term exposure to lung irritants or autoimmune diseases. Mesothelioma is specifically linked to asbestos exposure and involves malignant growth.
Similarities: Both pleural effusion and mesothelioma can cause fluid buildup around the lungs, leading to chest pain and difficulty breathing.
Differences: Pleural effusion can also be the result of heart failure, pneumonia or pulmonary embolism. Mesothelioma is specifically related to asbestos exposure.
Similarities: Pleurisy involves inflammation of the tissues around the lungs, causing sharp chest pain that worsens with breathing, similar to mesothelioma symptoms.
Differences: Pleurisy often results from infections, autoimmune conditions or lung diseases, while asbestos fibers irritating the pleura cause mesothelioma.
Because misdiagnosis of mesothelioma can occur, it’s essential to rule out other potential diagnoses. Accurate diagnosis requires thorough evaluation and often multiple diagnostic tests. Nurses should remember to consider mesothelioma, especially in patients with a history of asbestos exposure.
When assessing a patient for mesothelioma, nurses can better assess a patient’s risk factors and provide accurate diagnoses. Detailed questions about occupational, military and environmental exposure can help ensure you capture a thorough exposure history.
Effective communication and detailed questioning are essential nursing skills for identifying past asbestos exposures. Encouraging patients to share their entire exposure history can help ensure patients receive the attention and care they need based on their specific exposure risks.
When mesothelioma spreads or metastasizes, tumors can be found deeper in tissue or in nearby lymph nodes. Eventually the cancer can spread to more distant organs in the body or bones. Distant metastasis is a defining characteristic of late-stage or stage 4 mesothelioma.
In an interview with our Patient Advocate Dr. Snehal Smart, she advises focusing on the patient’s wishes when discussing mesothelioma stages. “I review quality vs quantity of life and how it’s a personal preference what a patient wants at their stage. If they want to pursue treatment, they have the option to talk to their doctor about chemo, immunotherapy or clinical trials,” she said.
Confined to the lining of one lung or the abdomen. Early detection allows for more treatment options.
Importance: Early detection can lead to more treatment options and better outcomes.
Nurse’s Role in Diagnosis: Encourage thorough initial screenings and consider surgical options.
Spread to nearby lymph nodes. Treatment options include surgery, chemotherapy, and radiation.
Importance: Treatment may include surgery, chemotherapy and radiation.
Nurse’s Role in Diagnosis: Emphasize the importance of imaging tests in identifying the extent of the spread.
Invasion of surrounding organs. Treatment becomes more aggressive, often focusing on multimodal approaches.
Importance: Treatment is often more aggressive and may focus on palliative care.
Nurse’s Role in Diagnosis: Discuss the likelihood of multimodal treatment approaches with patients.
Spread to distant organs. Treatment focuses on palliative care to improve quality of life.
Importance: Treatment is primarily palliative to improve quality of life.
Nurse’s Role in Diagnosis: Be honest and compassionate when discussing limited treatment options.
When mesothelioma cells move through the bloodstream or lymph system, this can significantly affect the patient’s prognosis. Late-stage mesothelioma often has fewer treatment options. Surgery and targeted therapy becomes less effective as tumors spread through the body.
Understanding the stages of mesothelioma is crucial for nurses, as it guides diagnosis and influences conversations about treatment and outcomes with patients. In our 2025 survey, 28% of respondents were unaware of their stage. Accurate staging allows for more tailored treatment plans, ensuring patients receive the best possible care tailored to their specific needs and circumstances.
I first remind patients that mesothelioma is very difficult to stage and to not focus on that number. There are better and more accurate ways to determine prognosis. The best advice is to first determine a treatment plan, then assess progression of disease over time to determine effectiveness and the response of treatment choice.

When discussing a mesothelioma diagnosis with patients and their loved ones, approach the conversation with sensitivity, empathy and honesty. Many patients report receiving their diagnosis with little hope and are often told to “plan their funerals,” which can be profoundly discouraging for them and their loved ones.
Tammy Frank, a peritoneal mesothelioma survivor we interviewed, was initially told she had only 6 months to live. She shares her story of resilience and recovery 25 years later, providing hope to others facing similar diagnoses.
“I found the best doctor out there. He gave me hope when I had none. Mesothelioma is not a death sentence.”
Some patients, like Susan Dickman, who was told she didn’t qualify for surgery, sought second opinions and found specialists willing to take on their cases. Susan’s determination led her to Dr. Edward Levine, who successfully performed surgery, and she now enjoys good health 12 years post-operation.
Communicating a mesothelioma diagnosis involves more than delivering medical facts. It’s about providing support, instilling hope and encouraging proactive steps toward treatment. Sharing survivor stories and emphasizing the importance of second opinions can empower patients to explore all possible avenues for their care.
Nurses and medical students should keep in mind many mesothelioma patients you’ll talk to are between the ages of 61 and 80. As you communicate with this population, take special care in providing information depending on the patient’s age, generation and cultural background.
Nurses should also be prepared to communicate primarily with family members or loved ones who serve as caregivers. In our State of Meso 2025 survey, up to 80% said they served as the primary mesothelioma caregiver at some point.
Mental health considerations among mesothelioma patients and caregivers should also be taken into account when developing your communication strategy. Rachel Thomas, a Community Mesothelioma Nurse Specialist, told the Royal College of Nursing: “It would be realistic to expect that many patients will experience anxiety and low mood at diagnosis and when treatment fails and their cancer progresses. But these may be short lived emotional responses to trauma or a life challenge.”
Thomas continued, “As clinicians, we need to be able to assess patients for psychopathological conditions such as anxiety and depression and ensure patients are signposted to the appropriate treatment if they are found to be experiencing one or more of these conditions.”
When patients are diagnosed with mesothelioma, they often have many questions about what their diagnosis means for them and what treatment options are available. As a nurse, being prepared to address these concerns with clear, compassionate responses can significantly alleviate their anxiety and help them make informed decisions about their care.
Dr. Smart says many patients focus on what happens after treatment, asking, “What will my quality of life be after surgery? Is it worth going through? What is the difference between immunotherapy and chemotherapy? Why would a doctor recommend chemo or immunotherapy over surgery? Will chemo or immunotherapy make me sicker than what I’m already feeling at the moment?”
Patients facing a mesothelioma diagnosis have many pressing questions about their health and future, but they may not know what to ask right away. Establishing clear and open communication with patients can help patients and their loved ones get more answers they’ll need as they process the diagnosis and consider what’s next.
Additional topics that may come up include what follow up tests a patient might require, other doctors they might need to consult or how to get a second opinion. Questions about available support or other resources may also come up as patients and their families consider costs and logistics of care.
To treat mesothelioma, health care professionals must consider various factors, such as the type and stage of mesothelioma, the patient’s overall health and treatment preferences. Developing an individualized treatment plan is crucial for effectively managing this complex disease.
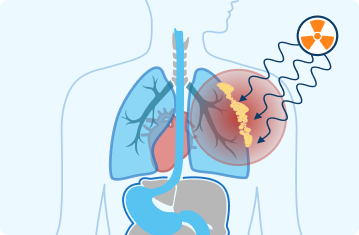
The main factors influencing mesothelioma treatment plans include the cancer’s location, stage and the patient’s health status. Mesothelioma often requires a combination of treatments, known as multimodal therapy, to maximize effectiveness and improve patient outcomes. This approach can include surgery, radiation, chemotherapy, immunotherapy and targeted therapy.
External Radiation: Uses high-energy rays to target and kill cancer cells in specific areas.
Surgery: Removes as much of the tumor as possible, often combined with other treatments to enhance effectiveness.
Chemotherapy: Uses drugs to kill cancer cells throughout the body intravenously or orally.
Internal Radiation (Brachytherapy): Places radioactive material inside or near the tumor.
Immunotherapy: Utilizes the patient’s immune system to fight cancer. Drugs like checkpoint inhibitors can help boost the body’s natural defenses to target and destroy cancer cells.
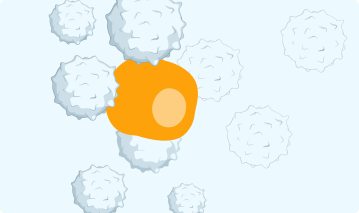
Targeted Therapy: Focuses on specific molecules and pathways involved in cancer growth. Examples include drugs that inhibit specific proteins or genes that promote cancer cell survival and proliferation.
A multimodal approach aims to control the disease and enhance the patient’s quality of life and overall prognosis. Nurses and other health care professionals can create a robust treatment plan tailored to each patient’s unique situation, understanding the various treatment modalities and how they can be combined.
If the patient is declining, they aren’t really looking for an action plan but want to know realistically how long this may go. Some spouses fear what the end stage will look like and want to know beforehand so they can start to prepare themselves mentally or emotionally for that.

Palliative care for mesothelioma focuses on alleviating symptoms and improving the quality of life for patients, regardless of their treatment choices. For instance, external radiation may be used to shrink tumors that cause discomfort, pleurodesis can alleviate fluid buildup in the chest and medications can help control pain and other symptoms.
A palliative approach can be integrated alongside aggressive treatments like surgery, chemotherapy or radiation therapy. It can also be the primary focus when patients decide not to pursue such interventions. Palliative care aims to address physical, emotional and psychological needs, providing holistic support to patients and their families.
Nursing and medical students must understand the principles of palliative care and how to deliver compassionate, patient-centered care. Teaching palliative care to students is essential for helping them feel confident and prepared, especially when dealing with their emotions and supporting grieving families.
Oncology nurses provide direct patient care, administer treatments and offer emotional support. They often work closely with specialists, physician assistants and residents. As a nurse, it’s also vital to communicate with social workers, physical therapists and dietitians to support patients’ emotional and practical needs.
Medical care for mesothelioma patients requires a comprehensive team approach, incorporating the skills and training of many health care professionals. Nurses assist oncologists, conducting physical exams, ordering and interpreting diagnostic tests and managing treatment plans. They are often patients’ primary point of contact, offering education and support.
Medical residents, under the supervision of attending physicians, gain hands-on experience, participating in surgeries, performing thoracentesis and other diagnostics procedures, administering chemotherapy and managing post-operative care. Pulmonologists and thoracic surgeons focus on respiratory function and surgical interventions.
Radiologists and pathologists also contribute significantly, with residents in these fields interpreting imaging studies and analyzing biopsy samples to confirm diagnoses and determine the cancer stage. A collaborative approach ensures that all aspects of the patient’s condition are thoroughly assessed and addressed.
Post-treatment life often includes regular follow-ups, managing long-term side effects and adapting to new routines. Understanding that recovery is a journey can empower patients and their families to embrace life after treatment with hope and determination.
Life after mesothelioma treatment can be challenging, but many survivors find ways to thrive and live fulfilling lives. Many survivors demonstrate remarkable resilience and hope through physical activity, advocacy or finding new purposes.
“It was good for me to talk with others with this disease. I know there were days at first, after the diagnosis, when I didn’t do anything and then went to bed feeling terrible. I could easily sit in my chair, staring at the TV and never move until I got up for another cup of coffee. But I realized you have to get past that, push yourself, and live your life. It makes you feel much better.”
Many survivors engage in support groups, participate in awareness campaigns and stay active to maintain their health. These activities help in recovery and provide a sense of community and purpose.
Patients and their families must understand that recovery involves managing physical health and addressing emotional and psychological well-being. As health care providers, it’s crucial to support and encourage patients in finding their path to a meaningful life after treatment.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Marchese, S. (2025, June 16). Mesothelioma Guide for Nursing & Medical Students. Asbestos.com. Retrieved December 18, 2025, from https://www.asbestos.com/featured-stories/student-guide/
Marchese, Sean. "Mesothelioma Guide for Nursing & Medical Students." Asbestos.com, 16 Jun 2025, https://www.asbestos.com/featured-stories/student-guide/.
Marchese, Sean. "Mesothelioma Guide for Nursing & Medical Students." Asbestos.com. Last modified June 16, 2025. https://www.asbestos.com/featured-stories/student-guide/.

Sean Marchese is a registered nurse with experience developing and managing respiratory oncology clinical trials and treatments. He has more than 10 years of clinical experience as a nurse in pain management, neurosurgery and clinical trials.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
