Your Guide to Types of Cancer Screenings for Every Age
Written by Karen Selby, RN
Breast Cancer Screenings
Breast cancer is the second-most common cancer for women. Each year, roughly 250,000 women and 2,300 men are diagnosed with this disease. Being vigilant about breast exams can help identify it early.
Types of Breast Cancer Screenings
The following tests are used to screen for breast cancer:
Mammography
The most common breast cancer exam is the mammogram. A mammogram is an X-ray of the breast that can identify the cancer before the patient is showing symptoms or feels a lump in the breast. Screening mammograms are used to look for signs of breast cancer in people who aren’t showing any symptoms, and should be given every few years. In the event an abnormality is spotted, a diagnostic mammogram will be given to identify the cause.
MRI
Though magnetic resonance imaging (MRI) is most commonly used for people who have already been diagnosed with breast cancer, a doctor may recommend it for people who have a high risk or family history of the disease. An MRI can provide in-depth images of the breast to give doctors information about the extent of the cancer, or a more detailed look to see if there are abnormalities present.
Clinical Breast Exam
A clinical breast exam is a routine checkup by a doctor to check for lumps in the breast. Although it’s best practice to perform these at home on yourself as well, a doctor may have more knowledge about what to feel for. These exams are often given during routine checkups by a gynecologist or primary care physician.
When Should I Be Screened for Breast Cancer?
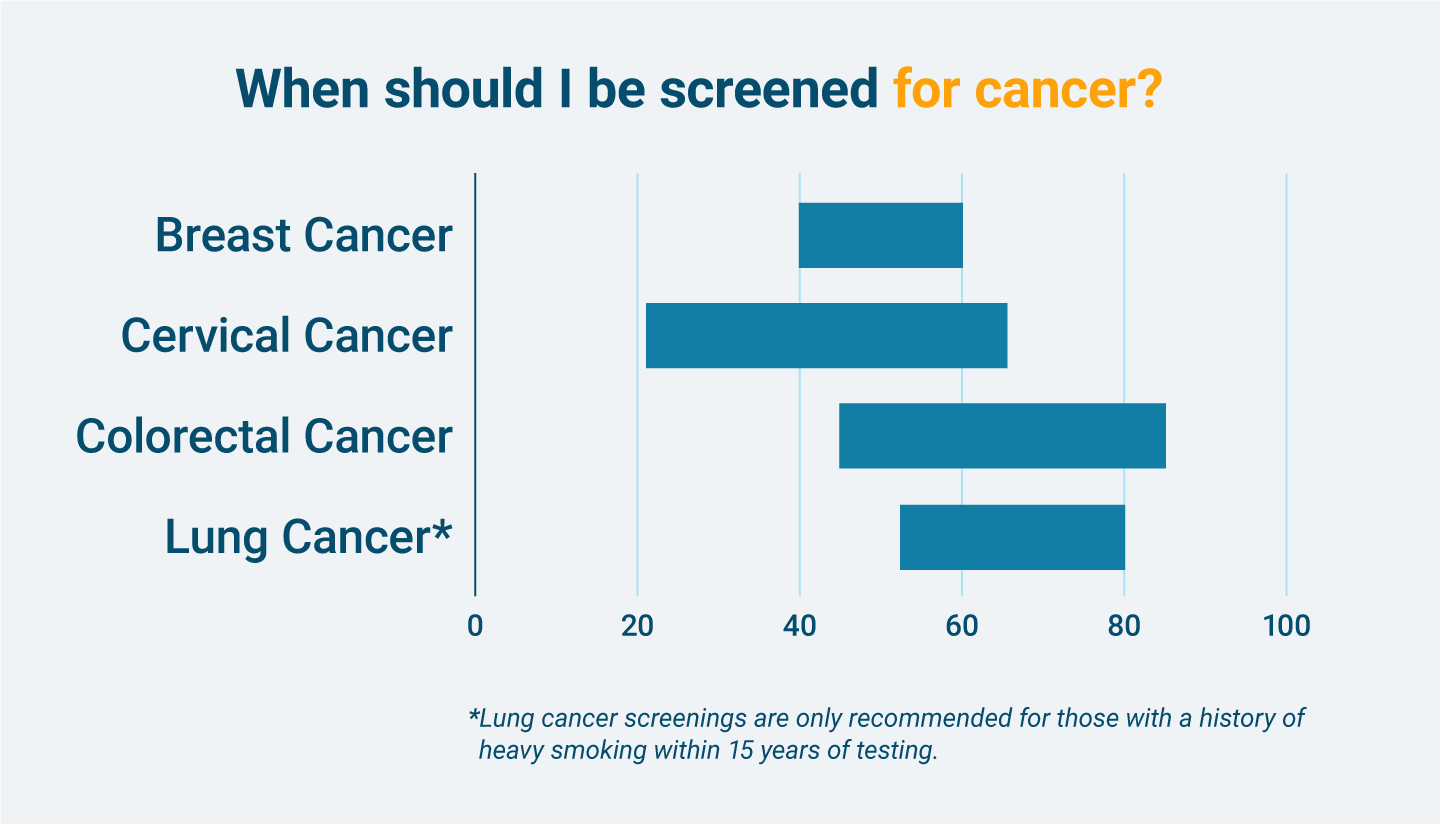
Self-assessment and clinical breast exams should begin as soon as you’re old enough to see a gynecologist. Once a woman is about 40 years old, she should begin getting a mammogram. The breast cancer screening guidelines are the following:
- Ages 40–44: Get a mammogram annually or every two years.
- Ages 45–54: Get a mammogram annually.
- Ages 55+: Get a mammogram every two years.
If you’re at high risk for breast cancer you should begin getting mammograms 10 years earlier than recommended for the general population, usually around age 30. Mammograms aren’t typically recommended for men, though a doctor may recommend a screening mammogram for men who are at risk of developing breast cancer.
Breast Cancer Risk Factors
Breast cancer is not uniform, meaning these risk factors aren’t a guarantee you’ll get the disease. However, these factors can increase a person’s risk of developing cancerous tissue and may mean you want to be more diligent about screenings.
- Age: Aging increases the risk of developing breast cancer. Most cases are diagnosed in people over age 50.
- Genetic Mutations: Some people inherit or develop mutated genes that put them at risk for the disease. These can be identified through genetic testing.
- Family History of Breast Cancer: Though breast cancer isn’t passed down from generation to generation, a family history of the cancer puts your body at a higher risk of developing it as well.
- Reproductive History: Those who started a menstrual period before age 12 or started menopause after age 55 are at higher risk for breast cancer.
Breast Cancer Symptoms
People who are diagnosed with breast cancer don’t always have the same symptoms. However, here are some warning signs to look out for:
- A new lump in the breast or underarm
- Nipple discharge that is not breast milk
- Any change in the size or shape of the breast
- Pain in the breast
- Thickening, swelling or irritation in the breast

Get help paying for mesothelioma treatment by accessing trust funds, grants and other options.
Get Help NowCervical Cancer Screenings
Cervical cancer used to be the leading cause of cancer death for American women. However, this is no longer the case due to screenings that can identify cervical precancer before it becomes cancer.
Types of Cervical Cancer Screenings
The following tests are used to screen for cervical cancer:
Pap Smear
The Papanicolaou test, or Pap smear, is a routine test done at a gynecologist’s office that involves collecting cells from the cervix to look for cell abnormalities or changes that could become cervical cancer.
HPV Test
The HPV test is performed the same way as a Pap smear, and also collects cells from the cervix to test for abnormalities. The HPV test looks for signs of the human papillomavirus, which can cause cervical cancer.
When Should I Be Screened for Cervical Cancer?
It’s best to start getting screened for cervical cancer as soon as you begin seeing a gynecologist. The general guidelines for cervical cancer screenings are the following:
- Ages 21–29: Begin getting Pap smear tests every three years.
- Ages 30–64: Begin getting Pap smears every three years, an HPV test every five years or a combination of both tests every five years.
- Ages 65+: You may be allowed to stop screening for cervical cancer if you have had normal results for several years, or have undergone a total hysterectomy.
Cervical Cancer Risk Factors
Most cervical cancer cases are caused by HPV. However, the following factors can also increase your risk of developing the disease:
- HIV: This virus makes it hard for your body to fight off sickness and can lead to cervical cancer.
- Smoking: Tobacco byproducts may damage the DNA of cervical cells and increase the risk of developing cancer.
- Taking Birth Control Pills for More than Five Years: Long-term use of birth control pills can increase your risk of developing cancer. This risk lessens the longer you are off birth control pills.
- Giving Birth to Three or More Children: Women who have experienced more than three full-term pregnancies are at a higher risk of developing cervical cancer.
Cervical Cancer Symptoms
Early stages of cervical cancer will most likely not cause symptoms. However, later stages may cause abnormal bleeding or discharge from the vagina.
Colorectal Cancer Screenings
Excluding skin cancers, colorectal cancer — cancer of the colon and rectum — is the third-most common type of cancer diagnosed in men and women.
Types of Colorectal Cancer Screenings
The following tests are used to screen for colorectal cancer:
Visual Tests
The most common visual screening is the colonoscopy, during which a long, thin tube is inserted into the rectum to check for abnormalities in the colon. A virtual colonoscopy constructs an image of the colon using X-rays.
Stools Tests
Stool tests involve analysis of feces to detect blood or abnormal DNA. Your doctor will provide you with a collection kit that you fill with a sample of stool, then send into a lab for analysis.
When Should I Be Screened for Colorectal Cancer?
For people of average risk for colon cancer, screenings should begin at age 45. The guidelines for colon cancer screenings are the following:
- Ages 45–75: Begin screening for colon cancer through either stool-based or visual tests as recommended by your doctor.
- Ages 76–85: Determine with your doctor whether or not to continue screenings, based on life expectancy and overall health.
- Ages 86+: You no longer need to screen for colorectal cancer.
Colorectal Cancer Risk Factors
Colorectal cancer risk increases with age. Most cases develop in people over age 50.
- Age: Age increases the risk of developing colorectal cancer. You should begin screenings at age 45.
- Bowel Disease: Inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis can increase the risk of colorectal cancer.
- Family History: Family history of colorectal cancer or colorectal polyps increase your likelihood of developing cancer.
- Genetic Syndromes: Syndromes such as familial adenomatous polyposis and hereditary non-polyposis colorectal cancer can increase your risk.
Colorectal Cancer Symptoms
Colorectal cancer doesn’t typically show signs. However, these changes may indicate you need to talk to your doctor:
- Blood in the stool
- Persistent stomach pain
- Unexplained weight loss
Lung Cancer Screenings
Although the most common cause of lung cancer is smoking tobacco, cancer can also be found in those who never smoked but were exposed to asbestos or radon. Because mesothelioma is a rare prognosis, there are no direct recommended screening tests.
Types of Lung Cancer Screenings
Lung cancer testing isn’t as common as screenings for other types of cancer. However, the following test is used in some cases:
LDCT
A low-dose computed tomography test can help screen for lung cancer, but it isn’t generally recommended unless the patient has heavy risk factors for the disease, such as long-term smoking. During an LDCT test, an X-ray will take detailed images of the lungs so doctors can check for abnormalities.
When Should I Be Screened for Lung Cancer?
LDCT tests are only recommended for people between 55 and 80 years of age who have a history of heavy smoking within 15 years of testing. A heavy smoker is a person who has a smoking history of 30 “pack years” or more.
A pack year means smoking an average of one pack of cigarettes per day for one year. To have a history of 30 pack years, you would need to smoke one pack per day for 30 years, two packs per day for 15 years or three packs per day for 10 years. LDCT tests are not recommended for those who don’t smoke, and therefore are not typically used to diagnose mesothelioma.
Lung Cancer Risk Factors
Heavy smoking is the most obvious lung cancer risk factor. Other risk factors include:
- Cigarette Smoking: Cigarette smoking is the leading cause of lung cancer.
- Radon Exposure: Radon is a naturally occuring gas that can cause lung cancer in people exposed to it.
- Asbestos Exposure: People exposed to asbestos in their workplace or home are at risk of developing lung cancer.
- Family History: Family history with the disease could mean you live in an environment where you are exposed to cigarette smoke, radon or asbestos
In contrast, mesothelioma is a rare diagnosis that affects roughly 3,000 people per year and is caused by asbestos exposure. Mesothelioma differs from lung cancer, but can develop in the lungs — this is known as pleural mesothelioma.
Lung Cancer Symptoms
Lung cancer symptoms are different for everyone, so it’s important to be cognizant of how you feel. Symptoms can include the following:
- Persistent cough
- Chest pain
- Wheezing
- Coughing up blood
- Fatigue
- Unexplained weight loss
Mesothelioma Cancer Screenings
There are four types of mesothelioma, which indicate the location of the tumor: pleural mesothelioma (lung), peritoneal mesothelioma (abdomen), pericardial mesothelioma (heart) and testicular mesothelioma (testes). While there aren’t screening recommendations for mesothelioma and no screening that can decisively identify it, if you have been exposed to asbestos there are several screenings for asbestos-related diseases, including:
- Chest X-ray
- Low-dose CT scan
- Spirometry
- Bronchoscopy
- Bronchoalveolar lavage
- Pulmonary function tests
Mesothelioma Cancer Risk Factors
Approximately 80% of people who are diagnosed with mesothelioma cancer have been exposed to asbestos. Mesothelioma risk factors include:
- Occupational Exposure: Those who work in blue collar jobs in high-risk industries such as construction are more likely to be exposed to asbestos. Other jobs with occupational exposure include power plant workers, auto mechanics and firefighters.
- Military Experience: Military members or veterans who served on ships that contained asbestos products are more likely to be diagnosed with mesothelioma cancer.
- Location: Individuals living in residential areas near asbestos mines or similarly contaminated areas have a higher chance of asbestos exposure.
Mesothelioma Cancer Symptoms
Symptoms of mesothelioma vary by type. However, common symptoms of the disease include:
- Shortness of breath
- Cough
- Pain in the chest or abdomen
- Fatigue
- Fever or night sweats
- Respiratory complications
- Muscle weakness
- Nausea or bloating
Mesothelioma symptoms can begin 20 to 30 years after exposure, meaning you should never stop being vigilant about your lung health.
Other Types of Cancer Screenings
There is insufficient evidence to recommend screenings for other types of cancers such as prostate, ovarian or skin. However, if you feel that there is an abnormality with your health or that you are developing symptoms of one of these diseases, seek advice from your doctor to determine a plan for diagnosis and treatment.
General Wellness Tips to Avoid Cancer
Though exposure to asbestos and a subsequent mesothelioma diagnosis isn’t the fault of the patient, there are ways to keep your body in good health to avoid other types of illnesses.
Eat Healthy
A healthy diet can help reduce cancer risk. Red meat, for example, is linked to an increased risk of colorectal cancer. Eating foods that are high in vitamins and antioxidants — and avoiding foods that are processed — can help your body ward off disease.
Exercise
Staying active can also help your body ward off illness. Committing to just two hours of physical activity per week can help you combat the cancer risk involved with being overweight.
Avoid Tobacco
Lung cancer is the leading cause of cancer death in the United States, and smoking is the leading cause of the disease. Avoiding tobacco can help prevent lung cancer as well as other cancers like mouth and throat, esophagus, colorectal and kidney.
Avoid Alcohol
Excessive drinking has been linked to cancer risk for six types of cancers: mouth and throat, voice box, esophagus, colorectal and breast. Limiting alcohol intake can help reduce this risk — for those who do drink, the American Cancer Society recommends men drink a maximum of two drinks per day and women drink a maximum of one.
Wear Sunscreen
Skin cancer is the most diagnosed type of cancer in the United States. You can prevent skin cancer by wearing sunscreen when you go outdoors and wearing protective gear like a hat and sunglasses.
You know your body best. Take care of yourself by paying attention to any changes and by alerting your doctor immediately if you notice something out of the ordinary such as a sharp pain or a lump. Undergoing routine cancer screenings can also help identify anything you miss in at-home tests and can help you catch cancer early.
Usually, however, this isn’t the case for mesothelioma patients. In the event you find yourself navigating a mesothelioma diagnosis, take care of yourself by finding a doctor who is right for you and can help you navigate your care plan.