Webinar Recap: Immunotherapy for Mesothelioma
The Mesothelioma Center’s latest webinar on immunotherapy explored how the treatment works, who makes a good candidate and a wealth of other topics. You can still register for a free recording if you missed the live session.
Our expert speaker for the immunotherapy webinar was medical oncologist Dr. J. Marie Suga from Kaiser Permanente Vallejo Medical Center in California. She discussed the latest developments in treating mesothelioma with immunotherapy.
We also heard from a panel of survivors who shared their treatment experiences and tips for those considering immunotherapy:
At the end of the webinar, the panelists answered questions directly from the audience in a Q&A session. Patients, caregivers and family members learned invaluable information, from the top immunotherapy drugs for mesothelioma to how patients can access the treatment.
Immunotherapy Drugs and Who Responds Best
Suga, leading the first topic, explained how immunotherapy works and the benefits for mesothelioma patients.
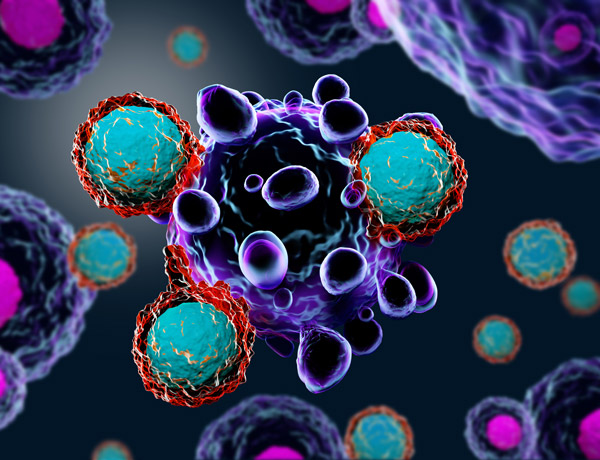
“Immunotherapy has exploded in oncology care. We’ve figured out that it’s a good option for many different cancers, including mesothelioma,” she said. “The goal of immunotherapy is to enhance your immune system’s ability to find the cancer. Almost anyone could benefit from immunotherapy. In any type of mesothelioma, it’s possible to get a response from treatment.”
Suga said there is a subset of patients who may experience a significant benefit from immunotherapy, particularly those with biphasic or sarcomatoid cells.
“There are two main classes of drugs: PD1/PDL1 inhibitor drugs and CTLA-4 inhibitor drugs,” she explained.
Nivolumab (Opdivo) is a PD1 inhibitor, and ipilimumab (Yervoy) is a CTLA-4 inhibitor. They are the two newest immunotherapy drugs approved by the U.S. Food and Drug Administration for mesothelioma. The FDA approved pembrolizumab (Keytruda) in 2020 as a second-line pleural mesothelioma treatment.
“It has a very similar mechanism to Opdivo,” Suga explained about Keytruda. “If you’ve been on Opdivo, most oncologists believe switching over to Keytruda would not be all that effective. One of the exciting things about immunotherapy is that sometimes the responses can be very long.”
Immunotherapy vs. Chemotherapy
One of the primary differences between immunotherapy and chemotherapy is symptom severity.
“The good thing about immunotherapy is it doesn’t linger. I’d be fatigued with chemotherapy for 10 or 11 days,” peritoneal survivor Randy Derouen recounted. He said he did have a slight reaction during treatment. “They slowed down the infusion rate into my body, and I never had any issues after that,” he said.
Immunotherapy can cause inflammation to any part of the body, and fatigue is common, according to Suga. She said that could be related to low thyroid levels. Derouen said chemotherapy was a different type of battle.
“Gradually, it just wore me down. It was a bit of a nightmare,” he recalled.
Suga explained that chemotherapy is designed to affect rapidly growing cells. “However, normal cells can also be affected by chemotherapy. That’s where the side effects normally come in and affect your skin cells or hair cells that rapidly turn over,” she said.
Derouen underwent a modified version of hyperthermic intraperitoneal chemotherapy, also known as HIPEC.
“I wasn’t a candidate for the full procedure because I had too much [cancer] next to my lower intestines,” he said.
Pleural mesothelioma survivor Michael Cole found success with immunotherapy in combination with radiation therapy.
“My doctor recommended we try targeted radiation with immunotherapy to weaken the tumors. We immediately saw that the tumors would slow to virtually a stop or slow growth rate,” he recounted.
Accessing Immunotherapy and What to Consider
“There are a lot of potential ways to get immunotherapy,” Suga explained to the webinar audience. “I always encourage people to look into whether there may be an appropriate clinical trial.”
Getting insurance coverage for immunotherapy with a peritoneal mesothelioma diagnosis can be more difficult. Derouen said he ran into problems.
“It’ll depend on the carrier itself. I probably would’ve looked at trials if it hadn’t been approved. I was just lucky it got approved,” he said.
The panelists emphasized that immunotherapy is an option to consider no matter what treatments you’ve had before.
“By the time we went to immunotherapy, we had pretty much exhausted all other options,” Cole said.
Suga explained there are many factors to consider when talking to patients about their treatment options.
“You have to weigh the pros and cons. A lot of that discussion is personal in terms of what treatments to try or what other options are available,” she said.
“There’s a lot of potential with where we go next,” Suga said when discussing the future of immunotherapy. “Knowing how much things have evolved over just a couple of years, things that are going to be game-changers in the future are happening right now. I think that’s really something to be encouraged about.”