Pleural Mesothelioma Survivor Shares His Inspiring Story

Fact Checked | Written by: Michael Cole | Last Update: 11/15/2024 | 7 Min Read
My story begins at the end of April 2015, when I went to my general practitioner’s office because of a cough and an unusual lack of energy. I thought maybe I was coming down with a case of pneumonia.
They listened to my chest, took an X-ray and told me to go straight to the hospital, where they quickly drained two liters of foul-looking fluid out of my right lung.
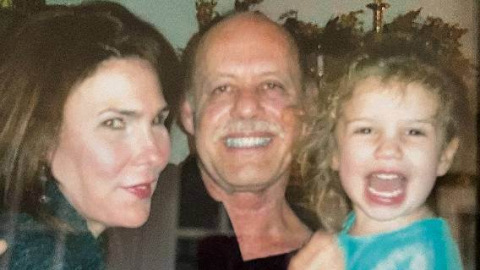
Four days later, Tania and I got the news: I had malignant pleural mesothelioma. The group of doctors in Fort Worth explained to us that mesothelioma is terminal, and I should not expect to live more than six months without treatment (they told my wife three months), and no more than three years with the best mesothelioma treatment available.
After they left the room, Tania and I were basically in shock. There was a feeling of smothering despair. What do we do? She grabbed her phone and looked up “mesothelioma.” No help there. It only made things worse.
After a few minutes she climbed up on the bed beside me and we prayed. I thanked God for our lives, my life, and everything he had done for us. We prayed that if I lived we would accept it, and if I didn’t we would accept that, too. We would trust him either way. When I say it felt like 10,000 pounds was lifted off my shoulders and the room brightened, I’m not exaggerating.
We discovered that one of the difficult things about the situation is how other people react to it. They have their own shock, grief, awkwardness, etc. Some just try to avoid it as much as they can. I don’t blame them.

Treatment Pioneer Dr. David Sugarbaker Steps in
The mesothelioma was advanced, and there was nothing that could be done, as far as they knew. However, one of the doctors there had previously worked in Boston with thoracic surgeon Dr. David Sugarbaker, a leading mesothelioma expert. He told us Dr. Sugarbaker had just recently moved to Baylor College of Medicine in Houston. We lived in Fort Worth, which is not exactly close, but at least is in the same state!
The thoracic surgeon asked if we would like for him to call Dr. Sugarbaker to ask if he would see me. We said of course, and he stepped out of the room. He returned after a couple of minutes. He had left a message. Within less than 10 minutes, his phone rang. Dr. Sugarbaker told him that he would be happy to see me.
My wife and I set an appointment to see Dr. Sugarbaker, and things moved fast from there. In May 2015, I had a surgical biopsy that confirmed the diagnosis, and we began to deal with all the new complications in our lives. What are we going to do about work? How will we get by financially? How can we afford to go back and forth to Houston? Where will we stay? All the while trying to deal with the emotional stress.
We saw a lot of lawyer ads at that time that said, “If you have been diagnosed with mesothelioma …” We received some compensation for mesothelioma. Every little bit helps, so we are thankful.
Mesothelioma Surgery Proves Challenging
We talked to Dr. Sugarbaker about our medical options. I told him I wanted him to “go in there and get all the cancer, everything he could see, and everywhere he thought it might be, or would go.” He looked relieved, and told me that if I were his brother, that’s exactly what he would want to do.
In June, I underwent an extrapleural pneumonectomy, also known as an EPP, the most aggressive mesothelioma surgery possible. As part of the procedure they removed my right lung, the pleural lining, the sac around my heart, the peritoneum lining around my stomach, some ribs, etc. They also used a hot chemo treatment in the thoracic cavity.
When I woke up I felt like I had been run over by a truck, and I’m pretty sure I looked worse. I had so many tubes and IVs either putting things in or draining stuff out. The IV stand looked like some kind of huge, demented Christmas tree. It was miserable.
I could have given up. I could have resisted or refused what the physicians and medical staff wanted me to do. For instance, I think it was the next day, maybe the day after, they told me I had to get up and walk. Believe me, the last thing I wanted to do was get up and walk. Especially with all those tubes, IVs, etc. sticking in and out of me.
They told me if I didn’t get up and move I would die. I still really didn’t want to, but I did it. It was misery. My whole body was out of whack, including my remaining lung. My pulse rate was around 165 at rest, and I could only take a few steps before I was winded. But I did it.
At first I had to push around a large, heavy walker. It was very stable and had places to carry the boxes that I was draining into. I called it the “dump truck.” A whole herd of people walked along with me. I think it took two to push my IV Christmas tree.
Over some days, the number of tubes, boxes, etc. reduced, and I was given a smaller, much lighter walker to push. I called it the “sports car.”
Pain and Stress Make Recovery Taxing
Things were looking up. Each day I could walk a little further, and a little further between stops to rest. I was in the ICU for about 10 days.
My wife was staying at a motel in the neighborhood. It was very difficult for her. A friend of mine whom I had not talked with for a while found out what was happening. He contacted my wife, packed his bags and came to Houston. He was such a blessing to us, both at that time and after.
The worst part of the surgery, for me, was the first day after they moved me out of the ICU to a regular room. I was having extreme pain in my right abdomen, and the medication they were able to give me outside the ICU was not controlling it.
That night, my pain went to at least a 15, on a scale of 1 to 10. I think now that it was the time my intestines and such tore their way through the webbing and moved up to where they are now – where the lower part of the right lung used to be. It makes sense now, but no one seemed to know what was happening then. I was a little miffed about that at the time, but the people on duty that day just didn’t know what to do, if there was anything to be done.
It hasn’t been easy, and we have been through hard times and uncertainty since that day, but don’t misunderstand. We have not been in despair. Tania’s support has been nonstop.
A friend of mine visited soon after my mesothelioma diagnosis. He has had cystic fibrosis since childhood, and every year for about the last 40 years they have been telling him not to expect to live more than a few more years.
He told me the biggest factor determining how long I would live would be my stress level and my attitude. His advice and encouragement helped a lot. Now, we encourage each other.