Berlin worked as a maintenance painter at a General Motors plant in Ohio. In 2009, he realized something was wrong. He was out of breath much too quickly. The dry cough and chest tightness were puzzling. Doctors diagnosed him with pleural mesothelioma. Berlin also was diagnosed with COPD, but he has learned to live with it, slowing his pace but hardly stopping him.
Chronic Obstructive Pulmonary Disease (COPD)
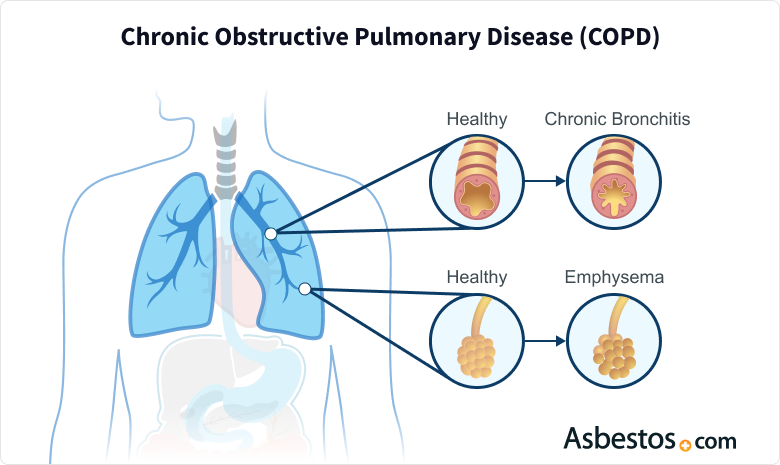
Chronic Obstructive Pulmonary Disease (COPD) is a lung disease that usually refers to chronic bronchitis and emphysema. Patients have difficulty breathing, and over time, the symptoms get worse. The main cause of COPD is smoking, but environmental toxins like pollution, chemical fumes, or exposure to workplace dust can also trigger the disease.
What Is Chronic Obstructive Pulmonary Disease?
People who have asbestosis, a lung disease caused by asbestos, may develop COPD as a complication. Asbestos is a cause of pleural mesothelioma, a cancer that affects the lining of the lungs. It is not uncommon for mesothelioma patients to also have COPD.
According to the U.S. Department of Health and Human Services, about 12 million Americans are diagnosed with COPD each year. An additional 12 million remain undiagnosed. This disease is the 4th leading cause of death in the U.S.
Generally, the disease is more common in people older than 40. Studies show that patients can expect to live 12-18 years after a COPD diagnosis, depending on the severity of the disease.
Typically, COPD develops slowly, and symptoms such as cough, increased mucus production, difficulty sleeping, shortness of breath, tightness in the chest and wheezing gradually worsen as the illness progresses. COPD affects the lungs’ elasticity, which makes it difficult for a patient to exhale correctly.
Complications include high blood pressure, heart attack and a higher risk of respiratory infections – including pneumonia, which can cause severe problems for COPD sufferers.
Correlation Between Asbestos and COPD

The inhalation of foreign fumes or substances can cause COPD. These irritants are often inhaled at the workplace. Asbestos materials were present at many industrial job sites. Workers who inhale chemicals, dust and fumes are at risk of developing COPD. Lungs that COPD weakens may also be much more susceptible to additional lung damage caused by asbestos.
Various scientific studies have reported a statistically significant incidence of COPD among those exposed to toxic materials such as asbestos and silica. Asbestos and COPD are associated, but research has not yet established a causal relationship.
A 2020 study published in Environmental Research and Public Health reported a marginal association between COPD and asbestos exposure among insulators. Researchers stated asbestos may cause airflow limitation in the presence of other substances, vapors, gases, and dust. The study also found that chest infections were significantly associated with asbestos exposure.
A Swedish study of 316,729 construction workers found the mortality rate from COPD was more than two and a half times higher in participants who had exposure to airborne toxins, including asbestos than in patients without exposure to toxic dust on the job. Exposure to inorganic dust even affected participants who had never smoked and were, therefore, at a considerably low risk of developing COPD.
Another study published in the Environmental Health journal in 2011 found that COPD caused by occupational exposure to dust or fumes caused about 375,000 deaths and 3,804,000 years of healthy life lost globally in one year.

Asbestos doesn’t directly cause COPD, but it can cause people to become more susceptible to the risk factors that cause COPD.
Symptoms
When someone first gets the disease, there may be few symptoms. Because COPD is a progressive disease, meaning it gets worse over time, symptoms typically worsen the longer someone has the disease.
- Cough with a lot of mucus
- Difficulty breathing or shortness of breath during physical activity
- Getting sick often with colds or the flu
- Lower muscle endurance
- Swelling in ankles, feet or legs (edema)
- Tightness in the chest
- Weight loss
- Wheezing
As the disease progresses, the air sacs in the lungs will expand less, and there may be more fluid and mucus in the lungs. This makes it increasingly difficult to breathe and get enough oxygen.
- Blue or gray lips or fingernails (signs of low blood oxygen)
- Difficulty breathing and talking
- Lack of mental alertness
- Rapid heartbeat
- Symptoms get worse
Over time, everyday activities like walking or climbing stairs can become challenging. Due to the strain on their heart and lungs, people with advanced COPD might experience chronic fatigue, weight loss and swelling in their ankles, feet or legs. Regular medical check-ups and early intervention can help manage symptoms and improve quality of life.
Diagnosing COPD

To diagnose COPD, doctors look at the symptoms, family history, medical history, and the results of special tests to measure lung health and function. The primary test used to diagnose COPD is called spirometry. Spirometry uses a spirometer to calculate the amount and speed of air the patient can blow out. The test is painless and non-invasive, and the patient blows into a tube connected to the spirometer. The doctor may also take another reading after giving the patient some medicine to help open the airways in the lungs to see how well the medicine works.
Using this test, a doctor can detect COPD before symptoms appear. It can also help doctors rule out other causes of symptoms, such as heart failure or asthma.
If you have been exposed to asbestos in the past and have been diagnosed with COPD, there may be a relation between the exposure complicating this disease. It is helpful to speak to your doctor about your exposure and to determine if your condition is a complication of asbestosis.
Image tests are also useful for diagnosing COPD. Using chest X-rays or CT scans, doctors can check the amount of damage in the lungs and rule out heart failure or other conditions.
Low blood oxygen is another sign of COPD. Doctors order an arterial blood gas test to measure the amount of oxygen in the blood. If it is too low, the patient may need oxygen therapy.
Doctors will stage COPD based on the severity of the damage in the lungs. This staging helps them decide on an appropriate treatment plan.

Receive a free guide with the latest information on emerging treatments and clinical trials.
Get Yours NowTreatment
Unfortunately, there is not yet a cure for COPD. However, several treatments can improve a patient’s quality of life and slow down lung damage.
- Lifestyle Changes: Quitting smoking, avoiding second-hand smoke or toxic fumes, eating a healthy diet with adequate nutrients, and getting safe levels of physical activity can improve symptoms and keep lungs from degrading.
- Medications: Bronchodilators are medicines that relax the muscles in the airways, allowing more oxygen into the body by making it easier to breathe. These are usually delivered through an inhaler. If the COPD is more severe, bronchodilators may be mixed with steroids in an inhaler to reduce inflammation. Doctors may also prescribe antibiotics to fight respiratory infections or steroids to reduce inflammation during flare-ups. Because people with COPD can have severe complications from respiratory infections, doctors recommend vaccines for the flu and pneumonia.
- Oxygen Therapy: This type of therapy increases the oxygen in the blood. Oxygen is delivered through nasal prongs or a face mask. Depending on the severity of the symptoms, oxygen may be used at certain times throughout the day or all day.
- Surgery: Many times, the air sac walls in the lungs are destroyed and create large spaces in the lungs called bullae. A bullectomy is a surgery that removes some of these spaces to reduce difficulty in breathing. Other surgeries involve removing damaged parts of the lung to help the lung work better. Lung transplants may also be an option.
Patients can adjust their home environment to make breathing easier. They should avoid cold or smoke-polluted air, and smokers are strongly urged to quit. Those with COPD may also benefit from joining a rehabilitation program or support group.
Recommended Reading




