Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

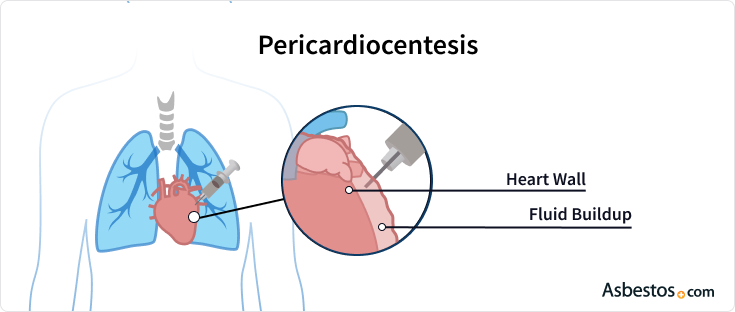
A pericardiocentesis is a procedure used to treat the buildup of fluid in the pericardium, which is the sac encasing the heart. Sometimes referred to as a pericardial tap, pericardiocentesis can help alleviate symptoms caused by pleural and pericardial mesothelioma.

A pericardiocentesis is a surgical procedure that removes excess fluid around the heart. The buildup of fluid in the heart lining is called pericardial effusion.
This can cause pressure on the heart, leading to dyspnea (shortness of breath) and coughing. The accumulation of too much fluid is dangerous because it can interfere with the heart’s functioning.
This procedure originated in the mid-1800s. By the 1900s, it was the preferred treatment method for patients suffering from pericardial effusion.
Pericardiocentesis was risky in the past without detailed imaging. But now that doctors can use ultrasound to guide them, it’s much safer. Although it’s not the only way to get rid of fluid around the heart, it’s usually chosen over surgery.
This procedure can ease symptoms and improve quality of life. Mesothelioma symptoms, including shortness of breath, coughing and chest pressure, may improve after the procedure.
Pericardial effusion can complicate cases of pleural and peritoneal mesothelioma and can also occur in very rare primary pericardial mesothelioma cases.
A 2021 study of a pericardial patient noted that pericardial fluid did not contain malignant cells. The diagnosis is difficult because tumor invasion of the myocardium may not appear on radiological imaging.
Although a pericardiocentesis cannot usually lead to a definitive diagnosis of pericardial mesothelioma, it can effectively treat symptoms of the cancer and potentially prevent further fluid buildup in the pericardium.
Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

A pericardiocentesis is performed in the hospital. It may take place in a room for surgery or a lab where special tools can check your heart. You may be requested to avoid eating or drinking for six or more hours prior to the procedure. Patients are often set up with an IV in case medications or fluids are needed during the procedure.
A doctor or other healthcare provider will clean an area near your chest and give you medicine to make it numb. A long, thin needle is then gently guided into the pericardial sac to draw out fluid. An echocardiogram, an ultrasound of the heart, is used to guide the needle and ensure there is no injury to the heart.
Once the needle is in place, it is removed and replaced with a catheter tube. The catheter drains the fluid into containers, sometimes for several hours or overnight.
Some patients feel pressure when the needle enters, and some people may experience chest pain, which is treatable with pain medication. Patients may also benefit from pain medication after the anesthesia wears off.
It’s best to ask your doctor what to expect after a pericardiocentesis. In general, you should be able to resume normal activities relatively soon after the procedure. However, you should avoid strenuous exercise or physical activity until your doctor says it is OK.
An additional echocardiogram can confirm the absence of fluid reaccumulation. An X-ray will ensure the needle did not puncture your lungs. Your medical team will closely monitor your vital signs, such as your heart rate, breathing and blood and oxygen levels.
After leaving the hospital, you should contact your doctor immediately if you experience increased draining from the needle insertion site, chest pain or severe symptoms.
Because it is performed near the heart and lungs, pericardiocentesis can cause risks, such as heart puncture or abnormal heart rhythms. To ensure no complications, you will be monitored for several hours after the procedure.
Potential problems that can occur during or after pericardiocentesis include:
These complications are rare and may vary depending on your age, overall health, and the severity of the pericardial effusion. You may need to have the procedure more than once, especially if fluid continues to accumulate in the area.

Eating the right diet throughout mesothelioma treatment can ease your symptoms.
Get Free Recipes and TipsA patient with recurrent pericardial effusions may receive several pericardiocentesis procedures. Chest X-ray and echocardiography can detect recurring pericardial effusions.
CT scans are sometimes capable of detecting pericardial mesothelioma tumors, but they often fail to detect diffuse mesothelioma tumors, which grow in a diffused pattern throughout the pericardium rather than as a solid mass.
Diagnostic testing of the fluid extracted—called effusion cytology—is commonly performed after each procedure. Doctors continue using pericardiocentesis for diagnostic purposes. However, according to a 2016 study from Hindawi’s Case Reports in Medicine, the procedure is diagnostic in only 25% of pericardial mesothelioma cases.
Pericardial mesothelioma is rare and difficult to diagnose. When mesothelioma is present, pericardial fluid does not usually contain malignant cells.
In most cases of primary pericardial mesothelioma, confirmation of diagnosis usually requires a biopsy of the tumor. A pericardiectomy is required to obtain a biopsy. This surgery can also relieve pericardial effusion and may prevent its recurrence.
This Page Contains 9 Cited Articles
The sources on all content featured in The Mesothelioma Center at Asbestos.com include medical and scientific studies, peer-reviewed studies and other research documents from reputable organizations.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, September 10). Pericardiocentesis. Asbestos.com. Retrieved January 16, 2025, from https://www.asbestos.com/treatment/surgery/pericardiocentesis/
Selby, Karen. "Pericardiocentesis." Asbestos.com, 10 Sep 2024, https://www.asbestos.com/treatment/surgery/pericardiocentesis/.
Selby, Karen. "Pericardiocentesis." Asbestos.com. Last modified September 10, 2024. https://www.asbestos.com/treatment/surgery/pericardiocentesis/.
Dr. Chuong Hoang is a thoracic surgeon researching mesothelioma surgical advancements at the National Cancer Institute in Bethesda, Maryland.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
Mesothelioma Center - Vital Services for Cancer Patients & Families doesn’t believe in selling customer information. However, as required by the new California Consumer Privacy Act (CCPA), you may record your preference to view or remove your personal information by completing the form below.
