Testicular Mesothelioma
Testicular mesothelioma is the rarest asbestos-related cancer. It forms in the lining of the testes. Symptoms include a buildup of fluid and painful swelling of the testes. The 5-year survival rate for testicular mesothelioma is 49%.
What Is Testicular Mesothelioma?
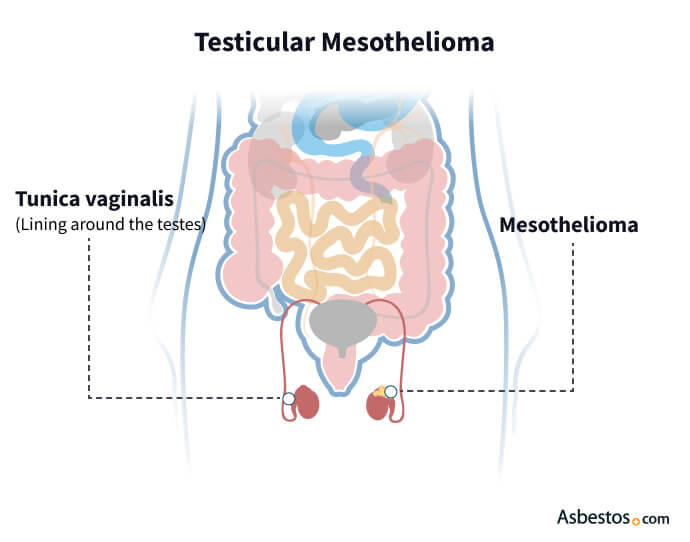
Testicular mesothelioma is a rare type of cancer that forms in the lining of the testes, known as the tunica vaginalis. Accounting for less than 1% of all mesothelioma cases, it is linked to asbestos exposure, similar to pleural and peritoneal mesothelioma.
- Like other forms of mesothelioma, asbestos exposure is a primary risk factor.
- Common symptoms include lumps, swelling, and fluid buildup in the scrotum.
- Diagnosis is challenging due to its rarity and symptoms that resemble more common conditions.
- Prognosis is generally more favorable compared to other mesothelioma types due to early-stage detection.
This form of cancer is difficult to diagnose due to its rarity, and symptoms often resemble other conditions, making it challenging for doctors to detect early. Despite the limited information, awareness of testicular mesothelioma continues to grow as more cases are studied.
Testicular Mesothelioma Symptoms
The most common symptoms of testicular mesothelioma are swelling or lumps in the testes, pain or discomfort in the scrotum, and fluid buildup, known as hydrocele. These symptoms can be concerning and similar to those of other, less severe conditions, such as hernias or infections. This overlap can lead to misdiagnosis or delays in receiving the correct treatment.
- Swelling or lumps in one or both testes.
- Pain or discomfort in the scrotum or testes.
- Fluid buildup in the scrotum (hydrocele).
- Change in the size or shape of the testes.
- Painful ejaculation or discomfort during sexual activity.
- Fatigue or unexplained weight loss.
It is crucial to seek medical attention if you experience any persistent symptoms, even mild ones. Early diagnosis is vital, leading to better treatment options and outcomes. If you or someone you know has a history of asbestos exposure and develops these symptoms, do not hesitate to consult a healthcare professional.
Causes and Risk Factors for Testicular Mesothelioma
Testicular mesothelioma is primarily linked to asbestos exposure, similar to other forms of mesothelioma. However, the direct connection between asbestos and testicular mesothelioma is not fully understood due to its extreme rarity. This cancer accounts for less than 1% of all mesothelioma cases, making research on its causes limited.
Asbestos exposure occurs when tiny fibers are inhaled or ingested, leading to serious health issues over time. Occupational risk factors associated with testicular mesothelioma. These include working on construction sites (carpenters), military jobs (veterans who served as mechanics, pilots, etc.) and industrial sites such as manufacturing, mining and shipbuilding.
In addition to asbestos exposure, other potential factors may contribute to the risk of developing testicular mesothelioma. These can include genetic predisposition or a history of different cancers, though more research is needed to understand these links fully. Given the rarity of testicular mesothelioma, awareness of these causes and risk factors is essential for early detection and prevention.
Doctors don’t yet understand how asbestos exposure can cause a primary tumor to develop on the tunica vaginalis. This area is the pouch of the serous membrane that covers the testes. Unlike pleural or peritoneal mesothelioma, this type does not only correlate to asbestos exposure.
Get specialized treatment from top mesothelioma doctors.
Find a Doctor NowDr. Jacques Fontaine, Pleural Mesothelioma Specialist

Diagnosis of Testicular Mesothelioma
Doctors often diagnose testicular mesothelioma during or after surgery because this type is rare and doesn’t present unique symptoms. The definitive way of confirming a mesothelioma diagnosis is to perform a biopsy.
This procedure involves removing a tissue sample from the tumor on the testes and sending it to the lab for testing. Immunohistochemical staining of the sample helps doctors determine if the patient has testicular mesothelioma.
Diagnosing testicular mesothelioma involves a combination of imaging tests and biopsies. Medical professionals often use several methods to identify this rare cancer, which can be challenging due to its similarity to other conditions, such as testicular cancer or benign cysts.
- Ultrasound: This test uses sound waves to create images of the testes. It helps doctors identify abnormal growths or fluid accumulation, which may indicate mesothelioma or other conditions.
- CT Scans: Computed tomography (CT) scans provide detailed images of the abdomen and pelvis. They can help detect tumors and determine if the cancer has spread to nearby lymph nodes or organs.
- Biopsies: A biopsy involves taking a small tissue sample from the testicle for laboratory analysis. This is the most definitive method for diagnosing testicular mesothelioma, as it allows doctors to confirm the presence of mesothelioma cells and distinguish the condition from other testicular issues.
Due to the rarity of testicular mesothelioma, many cases are often misdiagnosed. Symptoms may closely resemble those of more common conditions, leading to delays in accurate diagnosis. The biopsy is essential to rule out other testicular conditions. Health care professionals can better manage this rare cancer with the proper diagnostic approach and improve patient outcomes.
Treatment Options for Testicular Mesothelioma
The most common treatment for testicular mesothelioma is surgery. A 2023 research study noted testicular mesothelioma requires extensive resection, including metastatic surgery, if complete resection is possible. The study suggested a multimodality treatment plan for the malignancy, similar to a multimodal approach to pleural mesothelioma, offers the best patient outcomes.
Surgery may come before chemotherapy with cisplatin and pemetrexed, the longstanding standard-of-care treatment for mesothelioma. Doctors may offer radiation therapy next to kill any remaining cancer cells and prevent cancer from returning. Treating testicular mesothelioma requires a specialized approach due to its rarity. Treatment plans are tailored to the patient’s condition and factors like the stage of cancer, the patient’s overall health, and the potential for surgery.
- Radical Orchiectomy: This is the most common surgical treatment involving the removal of the affected testicle (orchiectomy) to eliminate the tumor.
- Debulking Surgery: In some cases, debulking surgery may remove as much of the tumor as possible, even if complete removal isn’t feasible.
- Chemotherapy: This treatment may be used post-surgery to target any remaining cancer cells, helping reduce the risk of recurrence.
- Radiation Therapy: For patients who may not be candidates for surgery, radiation therapy can be utilized alone or in combination with other treatments.
- Emerging Treatments: New therapies, such as immunotherapy, are being explored for their potential in managing rare cases like testicular mesothelioma, offering hope for more effective treatment options.
Considering the complexities of treating this rare cancer, consulting with a specialist is crucial for optimal management. In the 2019 study, only 5.3% of patients received radiation therapy. Given such a small group, researchers couldn’t determine if adjuvant therapy impacts overall survival.
In some cases, testicular mesothelioma is a secondary tumor, with the primary tumor located within the peritoneum (the membrane that lines the abdominal cavity). In these situations, doctors must treat the patient for peritoneal mesothelioma cancer.
Prognosis and Survival Rates for Testicular Mesothelioma
Testicular mesothelioma is extremely rare, making it challenging to gather comprehensive data on prognosis and survival. Prognosis refers to a disease’s likely course and outcome, while survival rates indicate the percentage of people who live for a specific time after diagnosis.
According to a 2019 study published in Urology, nearly 49% of patients survive 5 years after diagnosis, and 33% survive 10 years. The average life expectancy for testicular mesothelioma is between 20 months and 2 years. However, several factors influence these outcomes, such as the stage of diagnosis, the patient’s age and overall health, and the response to treatment.
Testicular mesothelioma patients I’ve spoken with are usually concerned about the rarity of this diagnosis. Some patients seem to have a longer life expectancy and better quality of life compared to patients with other types of mesothelioma.
Testicular mesothelioma is a clinically aggressive type of cancer, which means it can spread rapidly. While the testicular type tends to recur within a few years, even in cases where tumors are surgically removed, men with this cancer have a significantly better prognosis than most people with other types of mesothelioma.
Patients with the biphasic cell type had worse overall survival than other types. Of the 113 testicular mesothelioma patients in the study, 75% of cases had the epithelioid cell type. Older patients and those with tumors greater than or equal to 4 centimeters in size were associated with a worse survival rate.
Factors Affecting Prognosis
Understanding the factors influencing prognosis is crucial for patients diagnosed with testicular mesothelioma. While this rare cancer presents unique challenges, several vital elements can significantly impact outcomes.
Stage of Diagnosis
The stage at which testicular mesothelioma is diagnosed plays a critical role in prognosis. If detected early, patients typically have a better outlook when the cancer is still localized to the tunica vaginalis. Conversely, if diagnosed at a late stage, where the cancer has spread to nearby organs or lymph nodes, the prognosis is less favorable. Thankfully, many cases of testicular mesothelioma are diagnosed early due to its rarity, which can lead to improved outcomes.
Patient’s Age and Overall Health
Younger patients and those with good overall health generally respond better to treatment. A robust immune system can better handle aggressive treatments like chemotherapy and surgery. For example, patients under 50 often exhibit better treatment responses than older individuals. Survivor experiences often highlight the importance of maintaining good health throughout treatment.
Response to Treatment
The effectiveness of treatments, including surgery, chemotherapy, and newer therapies like immunotherapy, significantly impacts a patient’s prognosis. A positive response to initial treatments can improve survival rates and enhance the quality of life.
Monitoring
Regular follow-up appointments are crucial for tracking treatment responses and detecting early signs of recurrence. Monitoring can provide valuable insights into a patient’s progress and necessary adjustments in treatment plans.
By recognizing these factors, patients and their families can better navigate their treatment options and make informed decisions about their care.
Survival Rates for Testicular Mesothelioma
Due to the rarity of testicular mesothelioma, specific survival rate data is limited. However, studies suggest that 5-year survival rates can range from 50% to 60% when diagnosed early and treated promptly.
Comparison With Other Mesothelioma Types
Survival rates for testicular mesothelioma tend to be higher than those for other types of mesothelioma, such as pleural or peritoneal mesothelioma. This is primarily due to the localized nature of testicular mesothelioma, allowing for more effective treatment options.
Case Studies and Real-Life Examples
While comprehensive data on individual cases may be scarce, some patients have exceeded typical survival expectations through early detection and aggressive treatment. Sharing survivor stories can provide hope and insight into what is possible with prompt and adequate medical care.
Due to the rarity of this cancer, comprehensive survival data can be limited. However, studies indicate that early detection and prompt treatment can lead to more favorable outcomes. Understanding these testicular mesothelioma survival rates can empower patients and their loved ones as they navigate their treatment journey.
Commonly Asked Questions About Testicular Mesothelioma
- How is testicular mesothelioma different from testicular cancer?
-
Testicular mesothelioma specifically affects the lining of the testes, while testicular cancer originates in the testicular tissue itself. Both can present similar symptoms, but they are distinct diseases requiring different treatment approaches.
- What should I do if I have a history of asbestos exposure and testicular symptoms?
-
If you have been exposed to asbestos and experience symptoms such as swelling or discomfort in the testes, it is essential to seek medical attention immediately. Early diagnosis is critical for better treatment outcomes.
- Can testicular mesothelioma spread to other parts of the body?
-
Yes, like other cancers, testicular mesothelioma can metastasize or spread to nearby organs and lymph nodes. This is why early detection and treatment are crucial.
- Is financial compensation available for testicular mesothelioma caused by asbestos?
-
Yes, individuals diagnosed with testicular mesothelioma due to asbestos exposure may be eligible for financial compensation. It is advisable to consult with a legal expert specializing in asbestos-related cases to explore your options.




